Resilient Institutions: Learning from Canada’s COVID-19 Pandemic
Foreword
This report is a DIY project.
As the presidents of two organizations committed to better public policy and better government, we share a deep interest in what happened to our national institutions during COVID-19. During a pandemic-safe outdoor lunch in June 2022, we both noted there was no official effort to examine that key question on a pan-Canadian and public scale.
The Institute for Research on Public Policy’s Centre of Excellence on the Canadian Federation had already tried to step into the void of data by publishing a “stringency index,” collecting and disseminating information about the public health measures introduced in each province and territory. Government officials and researchers consulted these data regularly. Meanwhile, the IRPP’s online magazine Policy Options was inundated with submissions by experts eager to talk about the impact of, and how to respond to, the pandemic across a range of policy areas. The Institute also published a steady stream of research on the hard-hit long-term care sector.
David had unique insights into how provincial governments dealt with this unprecedented trial. As clerk of the executive council and deputy minister of intergovernmental affairs in Manitoba from May 2020 to November 2021, he had a first-hand view of the range of challenges, experiments and trade-offs that occurred during the pandemic. Now at the Institute on Governance, David wanted to draw out the governance lessons he and so many other public servants had applied so others could learn and benefit.
Therefore, it was through a combination of serendipity, curiosity and a desire to make a difference that we decided to organize a major conference and to publish a report based on what we heard.
If nobody was doing it, we would do it ourselves.
We really knew we were onto something when we started reaching out to potential participants for the conference, set for mid-June 2023 — typically, a very busy time of year. Yes, the invitees said overwhelmingly. An impressive roster of senior public servants, Indigenous and civil society leaders, politicians and other experts was assembled. Canadian scholar and author Alasdair Roberts, professor of public policy at the University of Massachusetts Amherst, signed on to give a keynote speech on “Building an Adaptable Country.”
What we heard was in equal parts frustrating and inspiring. The common feeling was that the pandemic experience was a singular opportunity for the country to make big changes and to build on lessons learned.
While many exhausted Canadians are ready to forget what happened, our leaders cannot — even if they try. Every day, they must deal with a suite of problems exacerbated by COVID-19 — including despairingly long health-care wait times, inflation and lingering public distrust of governments.
Yes, this report is a DIY project — and it is also a big nudge. With their resources, convening power, access to data and behind-the-scenes accounts, governments should take this conversation much further.
Jennifer Ditchburn David McLaughlin
President and CEO President and CEO
Institute for Research on Public Policy Institute on Governance
Executive Summary
The COVID-19 pandemic was a dramatic and unique moment in Canadian history. The impact might have been experienced differently from person to person and community to community, but the crisis experience was a collective one with which we are still coming to terms. Our key institutions were profoundly affected. They were forced to quickly change processes, forge new relationships or strengthen existing ones, and make pivotal decisions at an impossible pace with imperfect data.
There are critical lessons to be learned from that unprecedented time, knowledge that our institutions can apply to future crises.
That’s why the Institute on Governance (IOG) and the Institute for Research on Public Policy (IRPP) partnered to convene the two-day national Resilient Institutions conference in June 2023 in Ottawa. We brought together key decision-makers, practitioners and civil society actors who had been closely involved in the pandemic response to share experiences and ideas on how to make Canada’s institutions more resilient for the future.
We also scanned the national landscape for what other reviews had been done by different orders of government. This report is a summary and analysis of that research and the conversations from the national conference.
Four years after the shutdowns turned our lives upside down, this remains the only pan-Canadian study of its kind. But it is not enough.
How Did Institutions Fare?
We chose to assess four critical institutions: public health, the public service, federalism and democracy.
Our roundtable discussions revealed a mixed answer to the question of how Canada’s institutions performed but identified three broad perspectives:
- Canada’s institutions performed well, responding ably and agilely to an unprecedented situation.
- Canada’s institutions performed adequately with gaps and weaknesses that needed to be filled at the community level.
- Canada’s institutions performed poorly with inadequate and wrong responses that affected Canadians and reduced public trust.
The conference consensus was clear: Our institutions did not succeed completely, nor did they fail completely. The pandemic demonstrated how our institutions can be agile and nimble, but it also exposed some serious institutional and governance weaknesses that affected government responses and public health outcomes. Those weaknesses need to be addressed. While it is perhaps unsurprising that we heard a mixed review, it is important for decision-makers to consider the nuanced view that emerged on Canada’s institutional success. These three overarching perspectives are not mutually exclusive. Some institutions were described in successful terms at one moment during the pandemic and in less successful terms at another.
We heard about how Canada’s system of government was able to adapt to keep operating through unprecedented remote-work directives while pivoting to confront the pandemic. Public health measures were implemented quickly and relatively effectively in the first instance, which helped the country manage the onset of COVID-19. Canada’s vaccination program in 2021-22 was particularly successful. Public health co-operation and co-ordination across governments was particularly strong.
Indeed, intergovernmental relations were in many ways more successful during the crisis than in ordinary times. At the same time, we heard that these institutional successes were neither sustainable, due to the tremendous stress they put on the public-sector workforce, nor replicable in the absence of crisis conditions.
Successful outcomes were sometimes accomplished outside — or despite — these same public institutions.
Public institutions entered the pandemic with pre-existing capacity gaps and long-standing challenges, including outdated government data and IT systems and processes. Health-care systems were already operating under strained circumstances with significant human resources constraints, along with data-sharing platforms that were not optimally set up for a crisis.
We heard from community, local, cultural, Indigenous and other groups about the challenges they faced to be meaningfully included in decision-making. Then, we heard about the successes they had in reaching Canadians through tailored and culturally sensitive approaches — strongly suggesting that this should be normalized.
We heard that the pandemic impacted trust in our institutions generally and trust in public health institutions and public health officials more particularly. Perceived policy incoherence and the blunt nature of certain public health measures contributed to widespread pandemic fatigue. That was exacerbated by shifting scientific evidence and advice about how to respond to the virus itself and by inconsistent communication from public officials.
The pandemic shed light on, and worsened, certain relationships in the federation. The early positive tone of first ministers ultimately gave way to more typical arguments and recriminations. We heard about strains on the provincial-municipal relationship, as well as huge financial deficits faced by municipalities that are now on the front lines of addressing other crises, such as housing and opioids. There was also recognition that the health-care system does not serve everyone equitably and that this contributes to the health gaps that were experienced during the pandemic.
Lessons Learned and Recommendations
The report draws out four key lessons that capture the most significant learnings and makes 12 specific recommendations, which are addressed principally to governments and, by extension, all Canadians. They also touch upon civil society organizations and public policy stakeholders. Each recommendation forms part of what the country needs to do to ensure that we learn real lessons from the pandemic and act to make our institutions more resilient in the wake of it.
LESSON 1: INSTITUTIONAL CAPACITY CANNOT BE TAKEN FOR GRANTED
Much of the success of Canada’s pandemic response required individual acts of heroism such as public servants working overtime and creating new relationships on the fly, but this is not sustainable for the long term. To increase our institutional capacity, we make the following recommendations:
- Retool and reinvest in the public service’s digital and IT infrastructure.
- Create more integrated and efficient data-sharing pathways.
- Systematically examine the innovative processes and structures activated during the pandemic.
LESSON 2: THE INSTITUTIONS OF FEDERALISM WORK, UNTIL THEY DON’T
The intergovernmental infrastructure is largely driven by executive federalism, which excludes key actors such as municipal and Indigenous governments. To make the institutions of federalism more resilient, we make the following recommendations:
- Identify the processes and participants that worked best when it came to co-ordinating intergovernmental responses.
- Make intergovernmental relations more inclusive.
- Co-develop and formalize intergovernmental relations with Indigenous governments — a move that will require a shift to viewing them as governments, not just stakeholders.
LESSON 3: LEARNING TO NAVIGATE AND COMMUNICATE RISK AND UNCERTAINTY IS A PUBLIC SERVICE NECESSITY
Although the emergency phase of the pandemic is over, these factors permeate virtually every other potential future policy emergency — including climate change and natural disasters, future epidemics, etc. To better navigate this environment, we make the following recommendations:
- Incorporate positive risk-taking into public service processes to advance innovative ideas, improve service delivery and achieve better outcomes.
- Invest in the new leadership and operational skills development training needed and valued during the pandemic.
- Learn how to communicate policy uncertainty and complexity to Canadians.
LESSON 4: PUBLIC INSTITUTIONS CANNOT WORK WITHOUT PUBLIC TRUST
Public trust was deeply affected by the pandemic and we need to build it back or the next crisis will be infinitely more difficult to overcome. To rebuild this trust, we recommend the following:
- Create a pan-Canadian task force to tackle misinformation and disinformation and help governments understand how to mitigate disinformation/misinformation in future crises that require similar interventions.
- Build inclusive and meaningful relationships with civil society leaders before the crisis hits.
- The federal government should initiate a pan-Canadian comprehensive, collaborative lessons-learned examination that would systematically examine how our public institutions performed during the most demanding public health emergency of our time.
Conclusion
We recognize that we’re only scratching the surface. That is why many of our recommendations call for more to be done. Future studies and reports on Canada’s response to the pandemic should go above and beyond the public health dimension. A narrow health focus would be inadequate in capturing lessons learned. The same can be said for a narrow focus on government spending during the pandemic.
Canada’s COVID-19 response hinged on governance. That means there are key learnings to be drawn about how governments took decisions and who they involved; about how our federation works when governments must work together; and about how information flows within and across governments, and from governments to Canadians.
We hope this report acts as a call to action for governments and civil society to do more now before the natural inclination to “put this behind us” takes hold. It is crucial that our most important public institutions build resilience so they are ready for the next challenges.
Introduction
Those surreal weeks in March 2020 will forever be seared in our memory. Canadians were glued to TVs, radios and their phones, absorbing the news of how the “coronavirus” (as it was called then) was cutting a path of devastation through health systems around the world — and was now in Canada. Government leaders emerged to announce wide-scale shutdowns as part of their official COVID-19 response. Everything suddenly and drastically changed. It was a fearful, uncertain time for all Canadians.
Yet, Canada was not entirely unprepared. Following the 2003 SARS outbreak, Learning from SARS, a review conducted by the National Advisory Committee on SARS, led to new public health mechanisms and measures (Public Health Agency of Canada, 2003). These included the establishment of the Public Health Agency of Canada (PHAC) and the Federal-Provincial-Territorial Public Health Network Council as an intergovernmental forum for collaboration, co-ordination and governance. In 2016, federal-provincial-territorial (FPT) health ministers signed an information-sharing agreement on infectious diseases. The Canadian Public Health Laboratory Network, a network of federal and provincial public health laboratories, became a well-established mechanism to effectively collaborate on laboratory capacity-building and the response to emerging threats.
“Canada has made important gains in terms of our capacity to respond effectively to the public health challenges of serious infectious disease outbreaks. … Key lessons have been learned and milestones achieved that have shaped and sharpened our response approach and structures,” Chief Public Health Officer Theresa Tam wrote at the time of the 15th anniversary of the SARS outbreak (Tam, 2018).
Despite all this, Canadian decision-makers and health systems were overwhelmed by the rapid onset of COVID-19. Information on the virus and how to combat it was disjointed and unevenly applied. Its magnitude and virulence were underestimated and sometimes even ignored. Nothing, it seemed, had truly prepared Canadians for the long, difficult pandemic journey ahead. The toll was enormous, even if better than many countries. Approximately 4.6 million Canadians contracted COVID-19, and more than 51,000 Canadians died by March 2023. Canada’s mortality rate was 135 per 100,000 people by the same date. But some 72 other countries did worse (Johns Hopkins University, n.d.).
Yet, there has been no official, truly pan-Canadian “lessons-learned” commission or study post-COVID. That’s why the Institute on Governance (IOG) and the Institute for Research on Public Policy (IRPP) partnered to convene a two-day national conference in June 2023 in Ottawa. Our goal was to bring together key decision-makers, practitioners and civil society actors who had been closely involved in the pandemic response to share experiences and ideas on how to make Canada’s institutions more resilient for the future. As a result of these discussions, the IOG and IRPP have produced this report on what worked during the pandemic — and what didn’t — to assist governments in planning and delivering public services to Canadians in future crises.
We chose four critical institutions to assess:
- Public health
- Federalism
- Public service
- Democracy
The report focuses on selected key aspects of the pandemic response of each of these institutions. For public health, it was the nature of decision-making, and the availability and use of health data and information. For federalism, it was the early successes and later failures of intergovernmental collaboration, as well as the potential impact on federalism in the future. For the public service, it was internal decision-making, policy innovation, and the capacity and skills of public servants themselves. For democracy, it was the role of politicians and citizens and the impact of the pandemic on public trust.
While we had the generous co-operation of several current and former officials involved in the pandemic response across jurisdictions, we acknowledge that this report only scratches the surface of understanding Canada’s massive and complex institutional response to COVID-19. The conference and subsequent research should not be regarded as a proper substitute for a true national lessons-learned examination led by governments.
The pandemic challenged established conceptions of the role of government, the capacity of the public service, and the needs of the people they serve. Never has Canadian society been so riven by competing expectations of the role of the state and science while confronting issues of trust and disinformation. The collective unwillingness or inability to document what happened and why — including successes alongside the missteps — would be the biggest pandemic failure of all for Canada.
Where This Fits
The conference was not the first exercise to consider the response of Canadian governments to the COVID-19 pandemic. Several governments have conducted assessments and some are still doing so. Nevertheless, the extent of these exercises varies significantly, with many being relatively narrow in scope. Notably, they tend to fall short in comprehensively capturing the interdepartmental aspect, and even more so, the intergovernmental dynamics that unfolded during the pandemic, because these evaluations were predominantly conducted by individual departments on a specific element of the response and because most were done by auditors general. In addition, because these assessments were more often than not internal processes, the involvement of outside experts and larger communities affected by the pandemic was fairly limited, if not completely absent.
This is what the Resilient Institutions conference sought to remedy and where it is unique. It was the first exercise to bring together public servants and elected officials from different orders of government, as well as academics, health-care practitioners and community organizations.
Part I of this document provides a brief overview of reports produced by governments reviewing the pandemic response and describes the context in which the four institutions that were the focus of the event — health, federalism, public service and democracy — had to operate.
Government Reports About the COVID-19 Pandemic Response
It did not take long for some governments to initiate a review of their response — even while the COVID-19 pandemic was in full force. The first was published by Health Canada and the Public Health Agency of Canada in September 2020 (PHAC, 2020) before the second wave hit. Over the following months, the federal government, as well as provincial and territorial governments, conducted a series of reviews of different aspects of their responses. Importantly, the federal government has recently revealed that it has engaged the former chief scientific adviser of the United Kingdom to chair an expert panel to “…conduct a review of the federal approach to pandemic science advice and research coordination.” The aim is to “support Canada’s preparedness for future pandemics and health emergencies” (Government of Canada, 2023e).
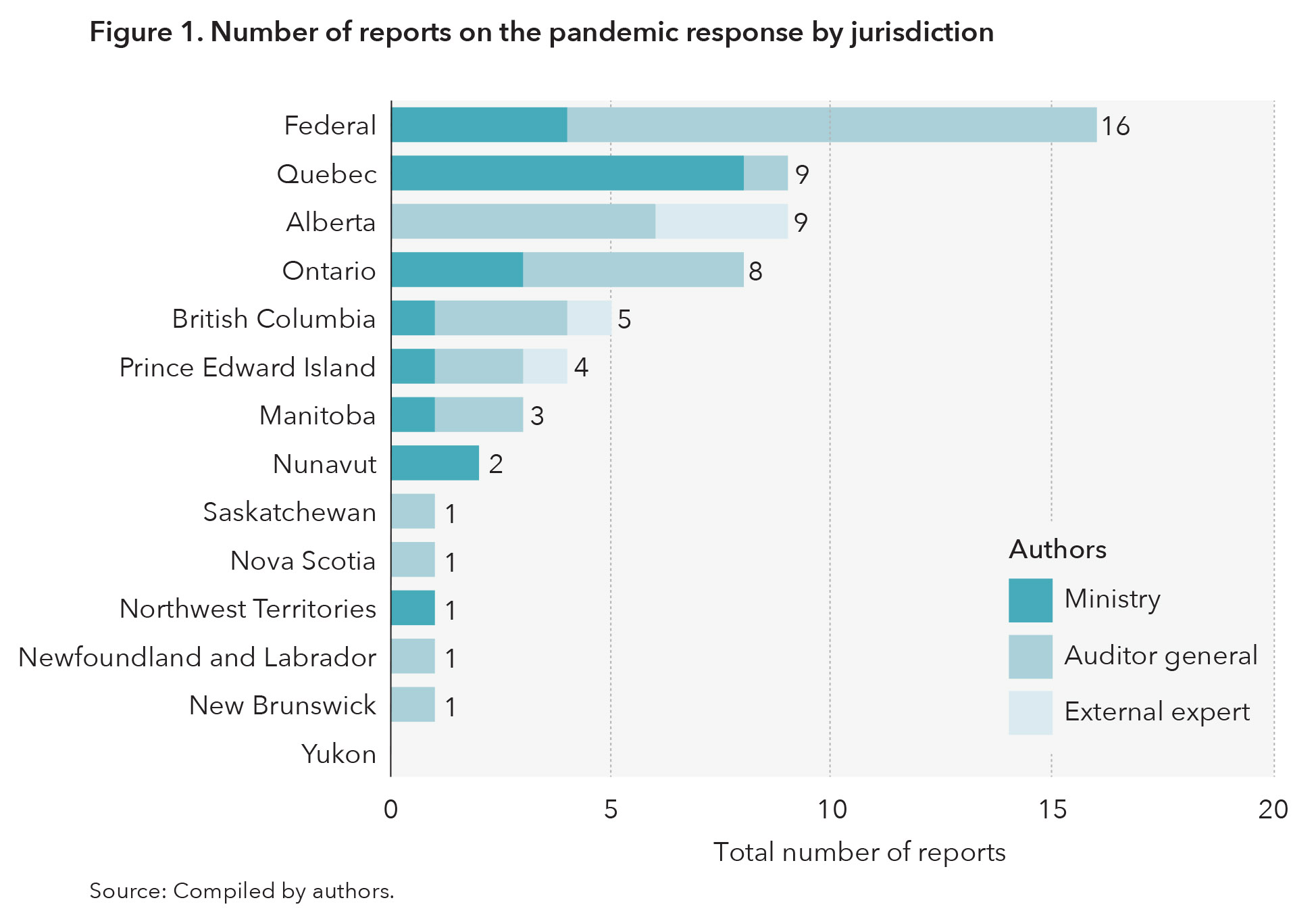
Figure 1 presents reports published by governments reviewing various aspects of their pandemic response (full list of reports in Appendix A). The reports are listed in three broad categories, based on who authored them: auditors general, departments or ministries, and/or external experts.
As the above figure shows, there is a wide variation in the number of public reports that federal and provincial governments produced. Importantly, 38 of the 61 reports captured in this review were written by auditors general. As expected, given their usual mandate, auditors general were tasked with determining if funds were appropriately distributed, with assessing the effectiveness of their distribution and with making recommendations for process changes pertaining to financial support in future emergencies. This was a more narrow, if crucial, review of lessons learned.
However, federal and provincial auditors general did not restrict their analyses to program spending. They also turned their attention to performance audits of pandemic programs. Performance audits of specific FPT programs differ from ministerial reports by also evaluating the effectiveness of a program or its economic or environmental impacts (Office of the Auditor General of Canada, n.d.) but not whether the programs were justified in the first place. These performance audits also determine whether the government had the means to monitor program results, then make recommendations based on their findings on these metrics.
For example, how provinces distributed vaccines was the subject of review by several auditors general. A British Columbia review looked at whether the provincial government was able to get the information it needed to monitor the overall provincial vaccination rate and the vaccination rates in long-term care homes and among health-care workers. The federal auditor general’s vaccination review evaluated whether procurement efforts by Health Canada and the PHAC were sufficient, whether access to vaccines across the country was efficient and if the two bodies were able to sufficiently monitor the distribution of vaccines.
The second type of reports was assessments produced by ministries or agencies on specific aspects of the pandemic. For instance, Quebec’s Commissaire à la santé et au bien-être produced six reports on what happened in long-term care facilities in the province. Quebec had the highest deaths per 100,000 in long-term care in the country in all first three waves of the pandemic (Canadian Institute for Health Information, n.d.-a), which perhaps makes this focus unsurprising. Many other provinces had significant outbreaks in their long-term care systems but did not scrutinize their response to the same extent. A report from the Quebec ombudsperson identified four key failings in the province’s response to outbreaks in long-term care homes:
- lack of sufficient infection-control strategies
- shortage of personal protective equipment (PPE)
- shortages of health-care personnel and related issues
- lack of support for mental health, social isolation and the importance of continuing access for residents to informal caregivers
Reports from the Commissaire à la santé et au bien-être in Quebec and the auditor general of Ontario also included a higher-level view and focused on the failure of governance in long-term care, such as systemic factors that culminated in poor conditions in the facilities and the lack of a reliable, quick data-collection system that made it difficult for decision-makers to have the important information needed to make policy decisions. The reports relied on interviews or surveys of health-care professionals to highlight some of the issues identified in addition to a review of documentation.
Seven ministerial reports included a record of all public health measures taken during the pandemic. Nunavut’s ministerial reports didn’t further analyze these health measures, while reports from the Northwest Territories, Ontario and the federal government used this as a starting point for improving their governments’ emergency preparedness plans. These reports were still ostensibly missing takeaways on the role of intergovernmental co-ordination going forward. The Northwest Territories collected feedback from decision-makers directly involved in the response, the public and Indigenous governments. Alberta, New Brunswick, Newfoundland and Labrador, Nova Scotia, Saskatchewan and Yukon did not produce ministerial reports or if they did, these were not made public.
Finally, the third type of review — those done by an external group of experts — is the one that was the most limited. We identified four of them, each with a very different format: three in Alberta and one in British Columbia.
In Alberta, the government commissioned KPMG, a professional services firm, to review the province’s overall response to the first wave of the pandemic, covering actions taken between March 1 and Oct. 20, 2020. The report was released in January of 2021. KPMG’s review was broad-based and looked at the acute-care response, continuing care response, engagement and communication strategies, procurement and PPE strategies, as well as governance and decision-making.
In 2023, Alberta also commissioned a report from a panel chaired by Preston Manning, former leader of the Reform Party. That report differed from the KPMG report by looking at “legislation and governance practices” (Manning et al., 2023, p. 5) during the pandemic. It included a public opinion component — an element missing from the KPMG report — by inviting the public to answer the question: “What, if any, amendments should be made to the legislation that governed Alberta’s response to COVID-19 in order to better equip the province to cope with future public health emergencies?” (Manning et al., 2023, p. 8).
Alberta also appointed an expert advisory panel to review children’s and youth’s well-being during the pandemic. That report was released in December 2021.
British Columbia commissioned a lessons-learned report from three former public servants who were tasked with undertaking “an operational review of the B.C. government’s pandemic response to help the government prepare for future events” (de Faye et al., 2022, p. iii). However, the approach and topics of interest between the B.C. report and the KPMG and Manning reports in Alberta differed substantively in composition and mandate, and the extent to which the public, First Nations and various stakeholders were consulted. The B.C. report also included recommendations on public trust of government, preparedness, implementation strategies and an entire section on Indigenous impacts. KPMG’s report for Alberta and the B.C. lessons learned reports looked at decision-making and communication strategies.
To summarize: Some aspects of the pandemic response have been reviewed by governments trying to identify lessons learned and to improve processes. But these have been intermittent and highly targeted. Certainly, no comparative or pan-Canadian review has been attempted. Although we can learn something from all these different lessons-learned reports, they leave large areas of the pandemic response unexamined, especially as it pertains to governments interacting with each other. In addition, the number of these exercises that were large in scope and encompassed various aspects of the different governments’ actions during the pandemic was limited, with nothing resembling the work of a comprehensive national review — something that others have urged (Bubela et al., 2023).
However, it is important to highlight that this short overview of governments’ assessments relies on publicly accessible content and therefore may potentially underestimate the depth and breadth of retrospective analyses, especially as COVID’s legacy unfurls. Notably, there has been nothing at the national level of common interest to all Canadians. We revisit this question in the lessons and recommendations section of this report.
The lack of comprehensive, public post-pandemic assessments by governments reinforced the importance of the Resilient Institutions conference. There was a particular need to bring together decision-makers, practitioners and observers from different jurisdictions who could share experiences that would reveal common or unique perspectives of deeper value than any single individual organizational or jurisdictional review. There was also a need to do so while events and actions were relatively fresh in people’s minds.
The Four Institutions
The conference created a unique opportunity to cultivate dialogue among various actors on four overarching institutions that were affected by, and relied upon during, the pandemic: public health, federalism, the public service and democracy. In addition to being central to the Canadian COVID response, these institutions are also the most important to be reinforced post-COVID. Below, we briefly summarize the context through which participants at the conference — each from one of these institutions — had to navigate during the pandemic, setting the stage for the conference’s discussions.
Public Health
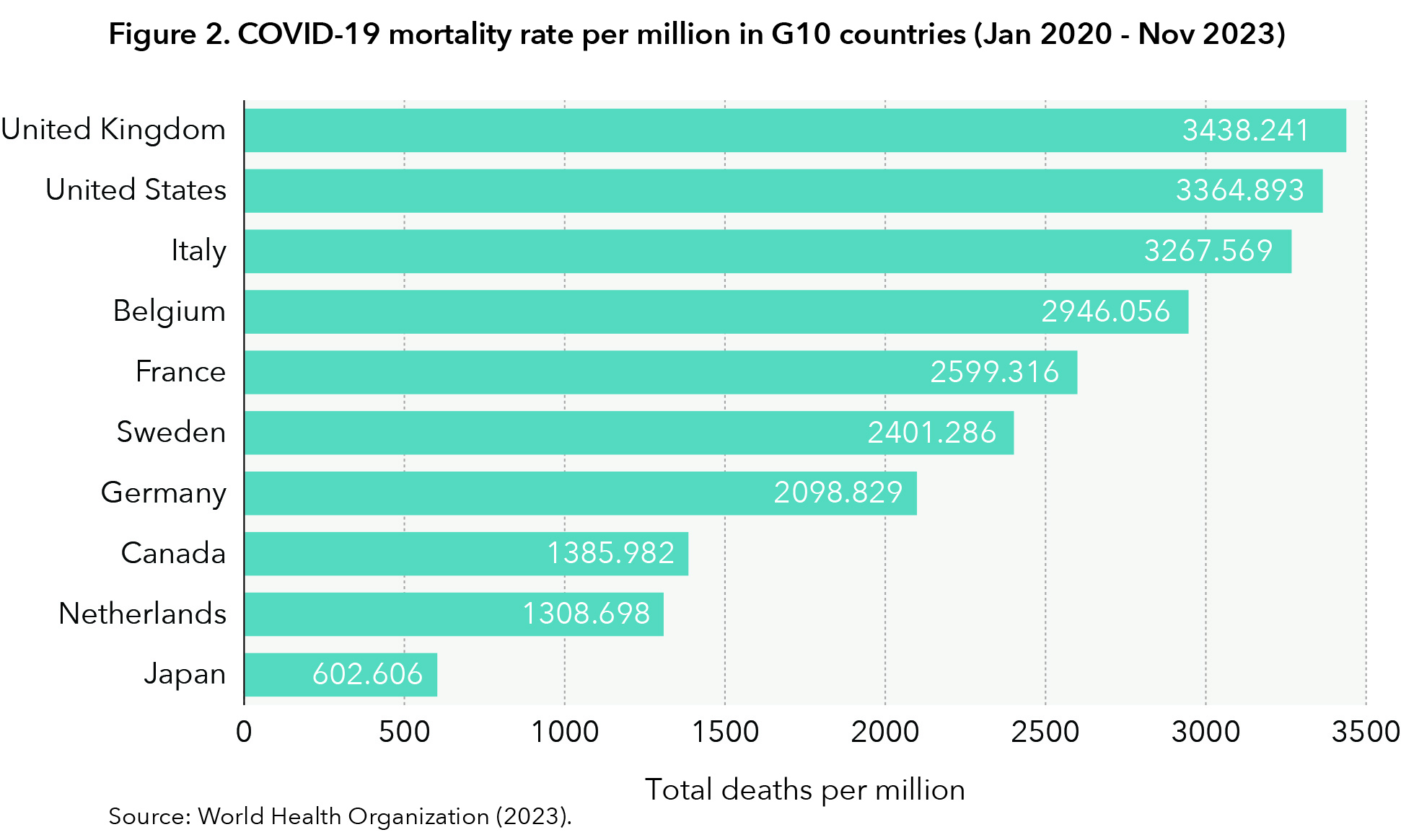
Helen Angus, former Ontario deputy minister of health, wrote in a commentary in Policy Options that “while not every decision was a good one,” Canada’s institutions worked largely as they were designed (Angus, 2023). Canada fared better than most G10 countries (apart from Japan and the Netherlands) for COVID-related mortality (Razak et al., 2022), as seen in figure 2.
However, as the pandemic spread across Canada, decision-makers faced long-standing structural challenges in health care and public health — chief among them a landscape that included a multitude of actors across jurisdictions who faced significant human and financial resource constraints, as well as barriers to data sharing.
Key actors in Canada’s pandemic response
At the federal level, decisions around the pandemic were primarily made through a cabinet subcommittee, which provided whole-of-government co-ordination and leadership. This committee was created on March 4, 2020, and worked in conjunction with the existing incident response group. The incident response group is an ad hoc working group of relevant ministers and senior government officials and was convened to discuss COVID-19 for the first time on Jan. 27, 2020 (Office of the Prime Minister, 2020). Additionally, the PHAC disseminated health information and guidance on the pandemic response at the federal level. It also disseminated pandemic advice and provided information to ministers through the federal-provincial-territorial (FPT) special advisory committee on COVID-19.
In January 2020, Canada put into place the federal/provincial/territorial public health response plan for biological events, which activated several committees and associated secretariats to facilitate the public health response (Pan-Canadian Public Health Network, 2023), summarized in table 1 below:
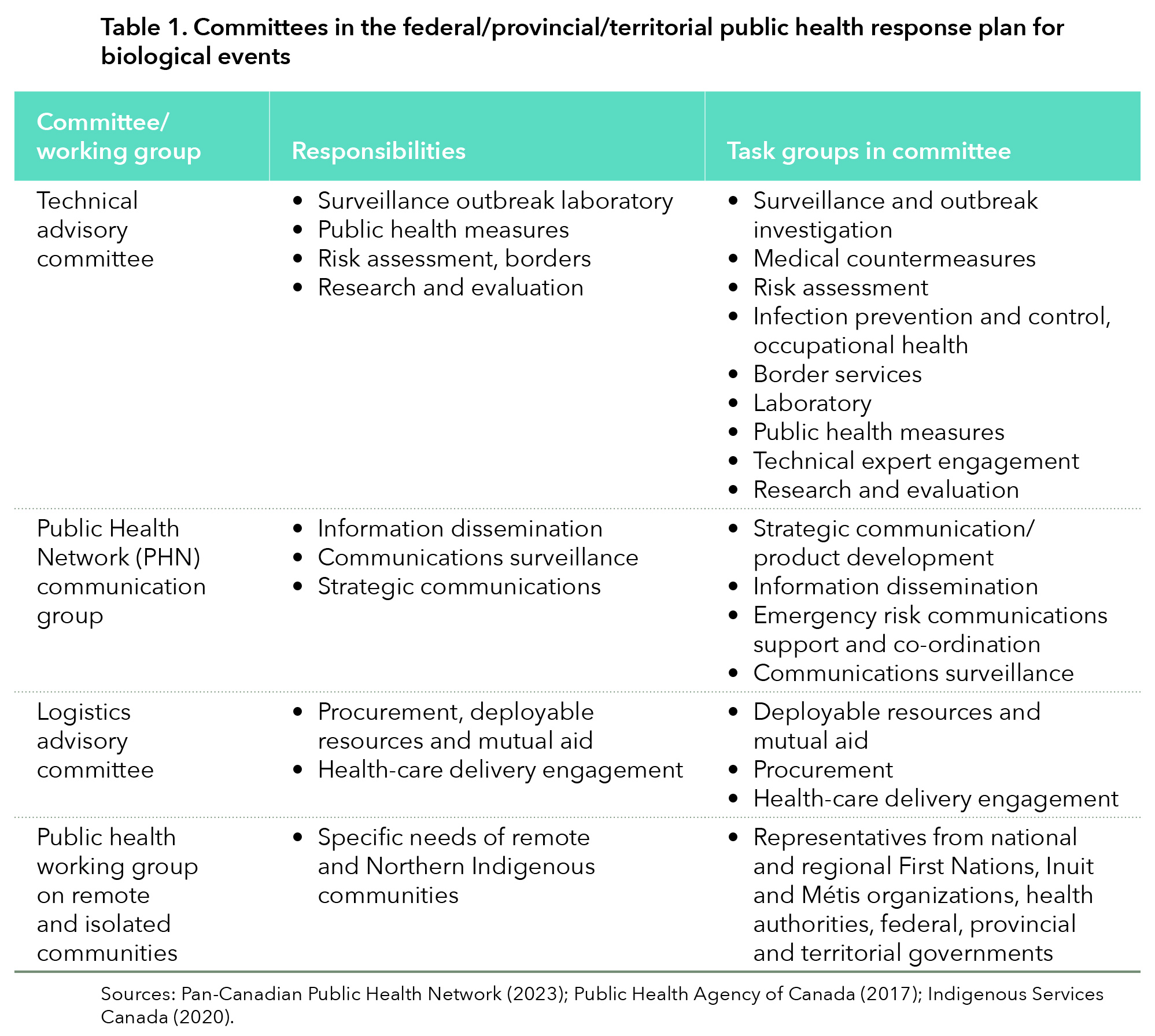
The committees in table 1 provided support to the special advisory committee that developed the federal, provincial and territorial public health response plan for ongoing management of COVID-19 (Government of Canada, 2022). This plan was not intended to serve as a list of obligations but instead laid out pan-Canadian considerations as governments transitioned out of the pandemic. For example, it included public health objectives, forward-planning assumptions and an overview of potential consequences of the pandemic response (Government of Canada, 2022).
At the provincial level, chief medical officers of health (CMOH) were key actors in the pandemic response. For many Canadians, CMOHs were some of the most visible public officials throughout the pandemic, appearing either independently or alongside premiers and ministers.
Crucially, the role of CMOHs is highly dependent on the institutional and legislative landscape and varies from one province to another. CMOHs can be placed along a continuum on two dimensions: their advisory capacity and their communication role (Cassola et al., 2022). In Canada, Cassola et al. (2022) identify three general models: technical expert, everybody’s expert, and loyal executive. These three models illustrate the range of reporting responsibility to the public and advisory responsibility to governments that CMOHs have.
As the pandemic showed, the CMOH role can evolve in response to or because of changes to legislation or relationship with the government, amongst others. For example, all CMOHs increased their communications to the public during the pandemic. Broadly, these communications fell under four themes: describing preparedness and capacity-building; issuing recommendations and mandates; expressing reassurance; and promoting public responsibility (Fafard et al., 2020). In addition to communications within their jurisdiction, CMOHs also periodically released joint statements through the Council of Chief Medical Officers of Health and exchanged information about the pandemic situation in their respective jurisdictions.
Resource constraints
Inadequate human resource capacity in health care is a core structural issue in Canada’s public health system. In general, Canada has fared average or below average across five metrics compared to its Organisation for Economic Co-operation and Development (OECD) peer countries. There are 2.8 doctors/1,000 population, lower than the OECD average of 3.7 doctors/1,000, and 2.6 hospital beds/1,000 population, lower than the OECD average of 4.3 beds/1,000 population. Canada’s performance on nurses per capita (10.3/1,000), is slightly higher than the OECD average (9.2/1,000) (OECD, 2023). The OECD does find that these capacity metrics are improving, except the number of hospital beds, which actually decreased over time.
Human capital is not the only resource constraint on public health capacity. The latest available data from the OECD show that, despite Canada spending US$6,319 per capita on health, higher than the OECD average of US$4,986 per capita (OECD, 2023), there are still long surgery wait times (Canadian Institute for Health Information, n.d.-b.), lack of access to a family doctor (CIHI, 2023) and emergency rooms at maximum capacity (Varner, 2023). For provinces and territories, health-care spending is the top expenditure (Statistics Canada, 2022a). Projections of demographic changes in Canada suggest health-care costs will rise as the population ages and requires more support across hospitals, long-term care homes, hospice care and in their communities.
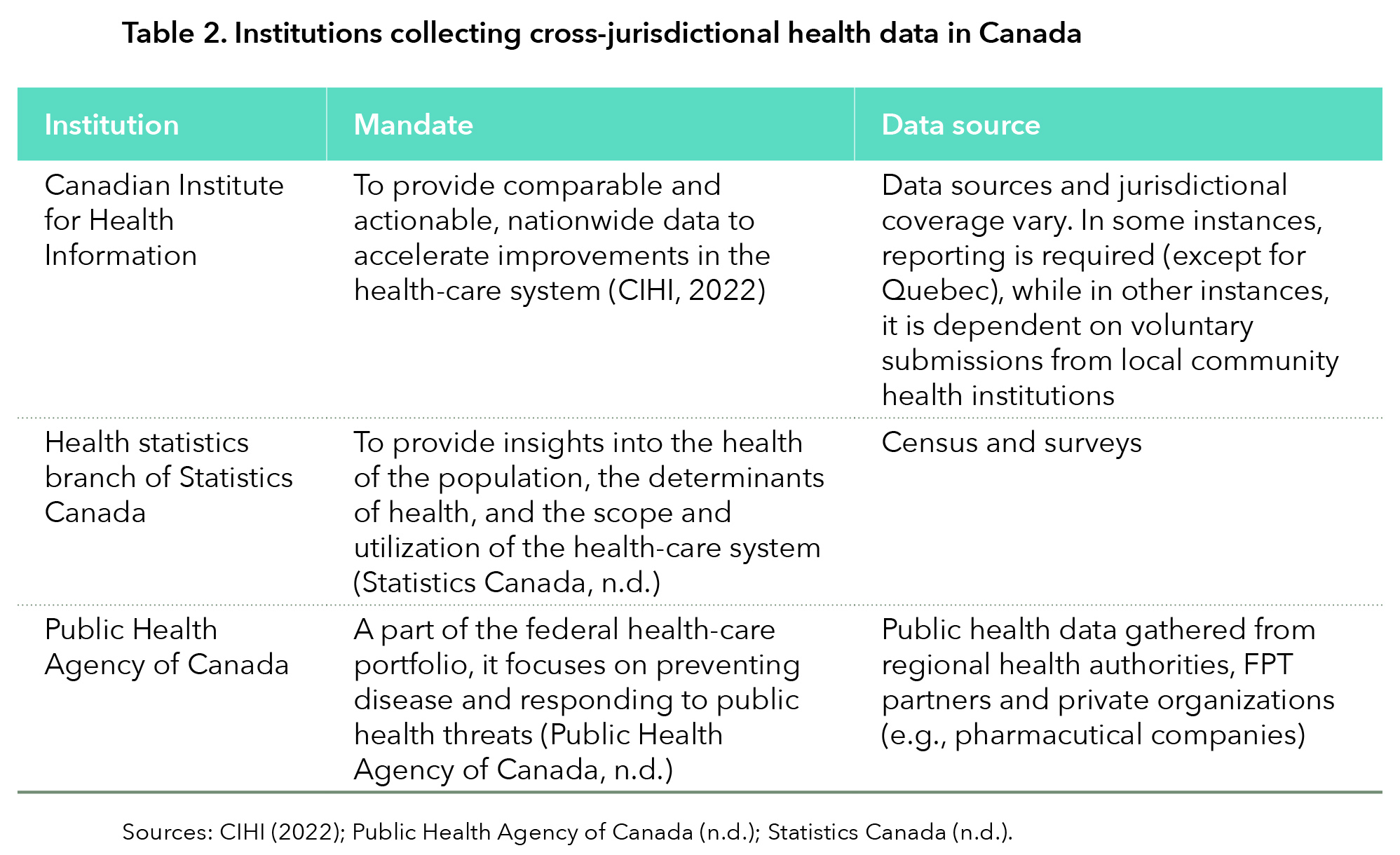
Data
Cross-jurisdictional data, such as administrative health data, are difficult to access in Canada because data governance practices differ from province to province. Many of the health data available are sourced from information collected by regional health authorities, surveys, and provincial and territorial departments. Statistics Canada and the PHAC are responsible for collecting and utilizing these data to create pan-Canadian databases for the benefit of policymakers and researchers on the governmental side, while CIHI is the only independent organization to do this work.
If pan-Canadian data are not aggregated by these organisations, decision-makers looking to make comparisons between provinces and territories must turn to provincial/territorial or regional sources. Each jurisdiction’s data are governed by a different institution. For instance, Katz et al. (2018) is a case study of the hoops through which researchers have to jump to access administrative health data. Their attempt to disentangle varying data governance systems across the country reveals a high administrative burden to access data across multiple jurisdictions. A key issue is how the institutional homes of administrative health data are different from province to province. For example, in Manitoba, provincial health data are housed at the Manitoba Centre for Health Policy at the University of Manitoba, which acts as a steward of information (University of Manitoba, n.d.). Conversely, in Alberta, administrative health data are collected and managed by a branch of Alberta Health Services. This barrier makes any jurisdictional comparison a resource-intensive endeavour.
Indigenous health care and data
Indigenous health care is funded, governed and delivered by both federal and provincial governments and in some scenarios by health authorities within Indigenous communities themselves. Within the federal government, Indigenous Services Canada provides direct funding of certain health services to First Nations and Inuit communities (Indigenous Services Canada, n.d.). Health Canada and the PHAC contribute to programs that support Indigenous Peoples living in urban settings or in Northern communities (Indigenous Services Canada, n.d.) Provinces indirectly support Indigenous health care because of their constitutional responsibility to implement health-care services for all inhabitants of the province.
In recent years, there has been a slow shift toward recognizing the inherent right of self-government for First Nations, Inuit and Métis, including when it comes to health care. This right has manifested in different ways across Indigenous communities. Most notably, in 2011, a tripartite framework agreement was signed by First Nations, the federal government and the B.C. government, leading to the creation of the First Nations Health Authority (FNHA) in 2013 (Indigenous Services Canada, n.d.), the first and only FNHA of its kind. The FNHA took over responsibility for programs previously administered by Health Canada (including direct provision of primary health care) and champions “culturally safe practices” throughout the broader health system (FNHA, n.d.). While this model has not been replicated in other provinces, there have been tripartite agreements signed to improve Indigenous governance of health care in Manitoba, Newfoundland and Labrador, Nova Scotia, Ontario and Quebec (Indigenous Services Canada, n.d.).
More attention was paid during COVID-19 to the impact on Indigenous communities than there had been during previous health emergencies. However, data availability was still poor and there is still no complete picture of how Indigenous communities fared, compared to their non-Indigenous counterparts. Instead, individual studies and information directly from Indigenous health leaders present a fragmented picture of the reality on the ground. One study found that, while infection rates were higher in non-First Nations individuals at one point during the pandemic, this dynamic flipped after Nov. 30, 2020, when COVID-19 began to spread to these communities (Mallard et al., 2021). Another study showed that mortality rates also followed this pattern (Tripp, 2022). Still, the lack of discrete health data for Indigenous populations before and during COVID-19 was a major hurdle to overcome in providing effective public health responses.
The availability of data on vaccination rates for First Nations people is slightly better than the information we have on Indigenous COVID-19-related infection and mortality. As of Sept. 5, 2023, the federal government reported that 93 per cent of First Nations people living on reserves had received their second dose and 40 per cent had received their third dose (Government of Canada, 2023a). There aren’t clear data for the overall rate of vaccination for Indigenous Peoples living off reserve. One study found that rates of vaccination for First Nations, Inuit and Métis people living in Toronto and London, Ont., were lower than city wide rates. Rates of vaccination (second dose) among First Nations, Inuit and Métis in Toronto were 58.2 per cent, and in London, 61.5 per cent (Smylie et al., 2022). For comparison, the overall rate of people who had completed their primary series[1] in Canada was 80.5 per cent (Government of Canada, 2023b).
Federalism
The pandemic made federalism real for many Canadians. For the first time, their ability to meet with their loved ones, leave their homes and even where they could shop depended on the province or territory in which they lived. There were similarities but many differences.
The Centre of Excellence on the Canadian Federation’s COVID-19 Stringency Index (figure 3) tracked these discrepancies by looking at public health measures such as school closures, business closures, vaccination passports and masking policies (Breton et al., 2021). In general, it found that most provinces experienced three peaks in stringency corresponding to their respective COVID-19 waves. However, the suite of measures used to control the pandemic differed from location to location, depending on governmental priorities. One example with significant variation was school closures. Some decision-makers argued that school closures should be a last resort, but the reality was that this was not always reflected in which measures provinces and territories chose to implement. A Policy Optionsarticle comparing school and restaurant closures found that provinces such as Ontario and Quebec had more days when restaurants were closed than schools, while provinces such as Nova Scotia and Manitoba had more days when schools were closed than restaurants, with other provinces falling somewhere between (Han & Breton 2022). The variability meant that Canadians across the country experienced pandemic restrictions in different ways.
But public health measures were just one part of the intergovernmental response to COVID. There were three main responsibilities of the federal government and federal agencies during the pandemic: providing guidance and direction for national co-ordination; control of international borders; and regulatory approval and procurement of the necessary medical supplies and vaccines (Public Health Agency of Canada, 2017). The federal government also created an FPT table for COVID-19 communications to facilitate dialogue between actors who may not normally exchange information, as well as to develop best communications practices, to spread information widely about the changing nature of the pandemic. Additionally, the federal government engaged external actors for feedback on communications efforts.
The federal government had responsibility for approving, procuring and distributing vaccines as well as other supplies to provinces and territories. This was a particularly crucial task because of the fierce global competition. As of July 14, 2023, 121,598,900 vaccine doses were purchased and distributed across Canada (Government of Canada, 2023c). Canada wound up with one of the highest vaccination rates in the world (Our World in Data, 2024).

The federal government also provided financial support of $19 billion to provinces and territories to mitigate stress on their health-care systems, to improve capacity for contact tracing and outbreak management, and to build out social services for Canadians through the safe restart agreement, which aimed to help provinces restore their economies (Government of Canada, 2020). Primary responsibility for the national economy rested with the federal government. It had the spending power to prop up livelihoods quickly and decisively.
The provincial and territorial governments’ responsibilities mainly centred around the provision of health-care services within their jurisdiction. The administration of some health systems was also delegated to regional or local public health units. For most Canadians, the provinces were the governments that had the most direct impact on how they experienced the pandemic. Given that this was a public health emergency, this is not surprising. Provinces were responsible for formulating and implementing public health restrictions; enforcement for schools and businesses; instituting limits on the size of gatherings; scaling vaccine administration; imposing travel restrictions; and masking (Public Health Agency of Canada, 2017). Provinces also took on the role of the main source of information about COVID-19 to their residents through daily updates from premiers, ministers of health and public health officials.
Mechanisms of co-ordination
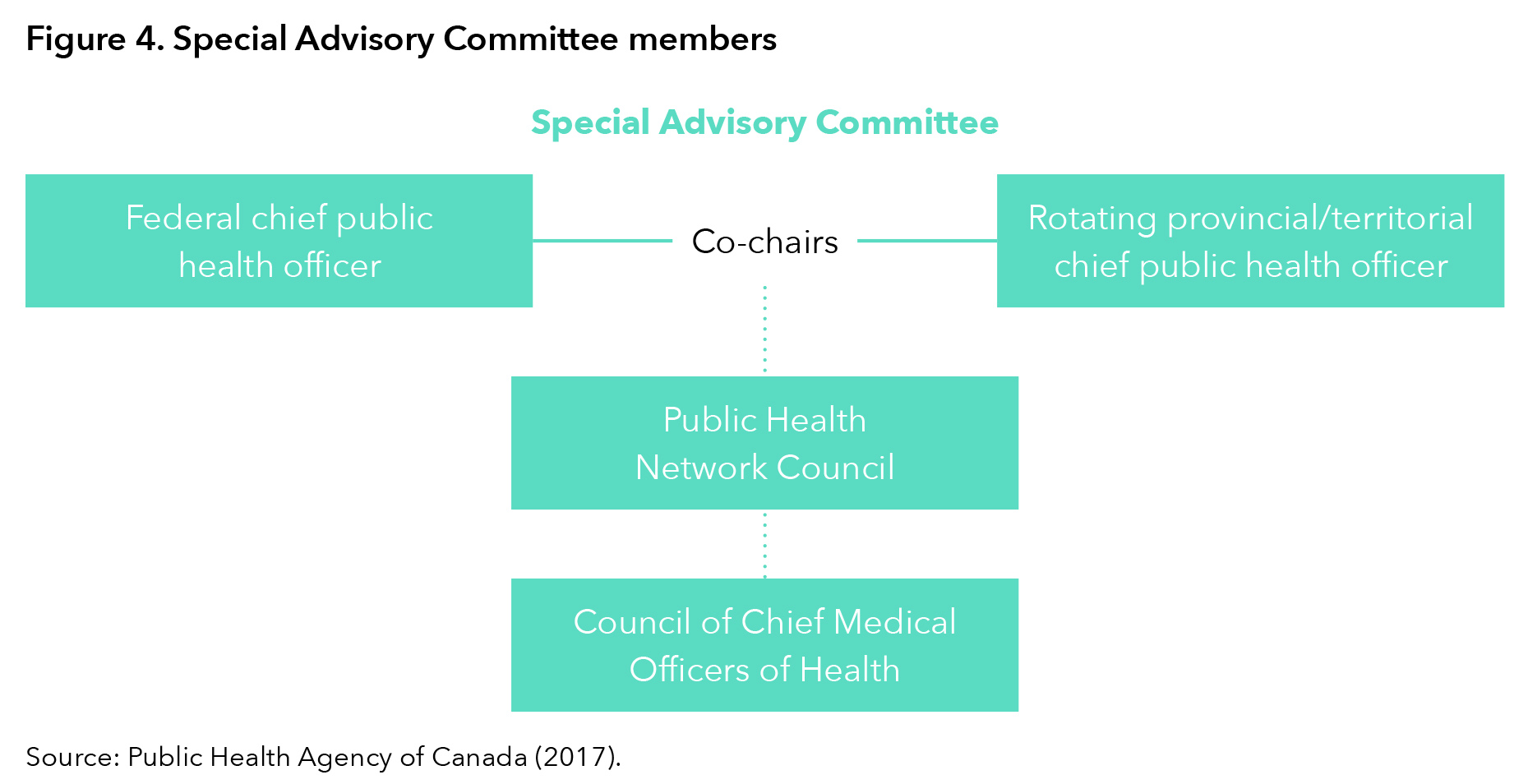
The pandemic required unprecedented levels of intergovernmental co-ordination to grapple with a virus that spread quickly across international and domestic borders. Co-ordination and information exchange between different jurisdictions happened mostly through informal (i.e., not constitutionally grounded), ad hoc forums. The division of federal, provincial, and municipal governments was laid out in the federal/provincial/territorial public health response plan for biological events. The plan includes a pathway for public health experts to give health advice to FPT deputy ministers of health through the special advisory committee (SAC). (See figure 4 for SAC membership.)
The federal-provincial-territorial relationship was co-ordinated mainly through first ministers’ meetings involving Prime Minister Justin Trudeau and the leaders of the 13 provinces and territories. While historically these meetings had been called on an ad hoc basis, they were called weekly during a significant portion of the pandemic. The exact number of meetings between the premiers and the prime minister during the pandemic is not publicly available, but the available numbers reinforce the heightened intensity in intergovernmental co-ordination during this time. As of Dec. 14, 2021, there had been 35 first ministers’ meetings (Office of the Prime Minister, 2021). Another avenue of intergovernmental co-operation on public health was a series of meetings of the FPT ministers of health and deputy ministers of health. As of November 2022, there had been 57 meetings of FPT ministers of health (Government of Canada, 2022).
The COVID-19 vaccination campaign was the largest mass vaccination campaign in Canadian history and exemplifies the elevated level of co-ordination and communication that was necessary between FPT governments. The federal government was responsible for procuring vaccines and for the regulatory approval of these new medicines. It had to make decisions about vaccine allocation between the 13 provinces and territories, as well as for Indigenous Peoples. Then, provincial governments had to make decisions about which jurisdictions should be prioritized and why; create plans for distribution; collect data around the immunization strategy; conduct community outreach; communicate emerging information about the vaccination to the public; and create strategies to combat vaccine hesitancy.
Other governments
Other orders of governments were central to the pandemic response despite being outside the core intergovernmental relationships described above. Municipal governments were often responsible for the first response to COVID-related policy implementation. While guidance and policy direction came from the provincial and federal levels, local health units were the figures on the ground involved in direct contact with the public. Municipal governments’ capacity to carry out policy direction was strained during the pandemic because they experienced extraordinary financial pressures due to the loss of revenue from changes in the population’s behaviour. For example, many public transit systems reduced service because of a migration of workers from the office to working from home — a shift that has been maintained in part long after the pandemic. Similarly, Indigenous leaders also bore responsibility for some aspects of policy implementation, with mixed degrees of support from federal and provincial governments. Panellists from our Resilient Institutionsconference argued that the lack of support was fuelled partly because of confusion from FPT governments about who was responsible for supporting Indigenous communities.
The Public Service
The public service was challenged more than ever by the pandemic. Almost overnight, governments across the country were faced with new priorities and an urgent need to adapt their ways of working. Citizen demands on governments increased and the crisis required the rapid development and rollout of various emergency relief measures and other public services. Only in 2024 is the last of these measures — small business loan support — being wound down. Frequent public communication and briefings from public servants to elected officials and the public became the norm. These impacts continue to be felt in the post-pandemic environment. As the deputy ministers’ task team on values and ethics noted in its 2023 report to the Clerk of the Privy Council: “The pandemic dramatically changed how the public service works, impacted citizens’ trust in public institutions, increased their expectations and diminished their overall satisfaction with government services” (Government of Canada, 2023d, p. 4). This is as good a summation as any.
Public service adaptations
There are numerous examples of the public service at several levels of government reconfiguring to meet the scale and nature of the crisis. What follows is a non-exhaustive sampling of some of those adaptations. In Ontario, the health command table, reporting to the minister of health, was set up to act as a single point of oversight and executive leadership for the province’s response. The province pivoted by adding more personnel to the Ministry of Health and other core ministries, adapting existing supply-chain work to focus on the procurement of PPE and increasing the Ministry of Health’s spending authority (Angus, 2023). Outside the health realm, the Ministry of the Attorney General pivoted by establishing a virtual court system to ensure continued proceedings (Adach, 2020).
The independent review of British Columbia’s operational response describes how the provincial government modified its approach to public service delivery. Employee resources were reallocated to support response programs, while ministries adapted to deliver some services online and rapidly made adjustments to maintain essential in-person service delivery. According to the authors, the task of configuring service delivery and providing necessary new services was “undertaken very rapidly, in days or weeks making changes that normally would take months or years to design and implement” (de Faye et al., 2022, p. 91).
The first volume of the New Brunswick auditor general’s performance audit on the pandemic illustrates how the government reconfigured typical executive council, cabinet and committee processes to get information more quickly to decision-makers and to facilitate rapid decision-making. The audit says: “The time required to bring information to decision makers was expedited from weeks, to at times, just hours” (Auditor General of New Brunswick, 2023, p. 33). This was achieved, among other measures, by assigning briefing responsibilities (which normally involved multiple steps and could take weeks) to the COVID core committee, a group of senior government officials, including the clerk of the executive council, the minister of justice and public safety, and the deputy minister of health (Auditor General of New Brunswick, 2023).
Manitoba experienced a relatively mild first wave of COVID-19, compared both to other jurisdictions and to what was to come. Pandemic responses were led by public health with an ad hoc committee of deputy ministers supporting it. Once the second wave of the virus became likely, a whole-of-government pandemic co-ordination response was deemed necessary. A COVID co-ordination committee (CCC) of all relevant departmental deputy ministers was established and chaired by the clerk of the executive council, including the chief medical officer of health, the chief nursing officer and other Manitoba Health representatives. This became the principal pandemic advisory and decision-making organ of the government. To facilitate ongoing cabinet engagement, several ministers were either invited or participated regularly to stay abreast of developments and to ask questions of officials. Daily CCC meetings were held, led off with a CMOH report on the state of the virus and health system impacts. Stand-alone task forces were established on testing, contact tracing, vaccination and enforcement to quickly ramp up the province’s capacity to respond to pandemic trends and developments. Information dashboards and COVID-19 modelling were regularly provided to the CCC. Health system representatives and Indigenous health services representatives attended, as required, to update participants on developments in their areas and to assist in co-ordinating responses.
What is clear in each of these examples is that existing governance structures and processes were inadequate to address the scale and scope of an effective pandemic response. New ones had to be created and old ones adapted to manage through this new reality.
Public servant adaptations
Public servants themselves faced new demands and demonstrated incredible dedication to tirelessly deliver services for Canadians (Wernick, 2023). These efforts took place in an entirely new working reality. On March 13, 2020, a work-from-home order for most federal public servants came into effect. The federal government rapidly modified its 1999 telework policy, then issued several new policies and directives in the two years that followed, including an easing of restrictions that led to the adoption of hybrid work models (Champagne et al., 2023). Prior to the pandemic, work-from-home had been limited, so the federal government needed to dramatically and rapidly enhance its remote work capabilities, such as increasing bandwidth, creating platforms for communication and enabling remote access, including for sensitive information (Shared Services Canada, 2021). Similar approaches were taken at different levels of government.
The unprecedented working reality undoubtedly took a toll on the public servants themselves. Burnout in the federal public service had previously been noted as a challenge and some studies pointed to a rise in burnout corresponding to the pandemic period (May, 2022). A 2021 study of the psychological health of a sample of Statistics Canada employees by creating a typology of psychological health and work engagement profiles found that 15 per cent of employees were “thriving,” 34 per cent were “doing well,” 38 per cent were “moving along” and 13 per cent were “struggling” (Blaiset al., 2023).
Long-standing challenges
Public services across Canada entered the pandemic facing a host of pre-existing institutional challenges. Public administration expert Amanda Clarke points to long-standing issues in the federal public service, including over-engineered processes, risk aversion, limited collaboration and outdated corporate policies related especially to IT and HR (Clarke, 2023). These factors would prove to be additional barriers that civil services needed to overcome when faced with the COVID crisis. They loom large in influencing how governments could, and did, respond to the pandemic.
Democracy
The pandemic had a profound impact on Canada’s democratic institutions, social discourse and trust in public institutions. The early days of the crisis were characterized by cross-party collaboration, public solidarity and a collective commitment to “flattening the curve.” Politicians worked across party lines to pass relief measures for Canadians while fear of the virus contributed to a period of high trust in elected officials (Turnbull, 2023). None of this lasted, however, as tensions arose around vaccination procurement and dispersal, mask mandates, lockdowns and the resultant disruptions to life and work. The political peace and collegiality that saw Canada through the first stage of the pandemic deteriorated as fatigue with pandemic measures set in and people became increasingly frustrated with what they saw as unnecessary government intrusion. Shifting information on both the virus and what to do about it contributed to this rising frustration.
Tensions culminated in the convoys and blockades in Ottawa and elsewhere during which public health measures were decried for their impact on individual freedoms. Although the number of actual participants in these activities constituted a very small percentage of the population, an Ekos Research poll found that 25 per cent of Canadians supported the convoy’s stated goals. However, it also found a positive correlation between support for the convoy and high levels of disinformation and mistrust (Ekos Politics, 2022).
The COVID-19 pandemic period both created and exacerbated social divisions. For example, higher earners were more likely to hold “pandemic-resilient” jobs that could be done remotely as compared with lower-paying jobs that experienced high volatility during the pandemic (Statistics Canada, 2022b). People’s trust in one another also varied along socio-economic lines. A study by Wu et al. found that peoples’ social trust, or trust in others, increased between 2019 and 2021 for those in higher socio-economic brackets and decreased for those in lower socio-economic positions (Wu et al., 2022).
Public trust
Public trust was a key factor in ensuring adherence to public health measures, but levels of trust were by no means stable throughout the crisis. In their Policy Options article commissioned for the conference, McAndrews et al. trace the evolution of public trust in institutions, specifically examining whom Canadians trusted to provide them with reliable information about the pandemic (McAndrews et al., 2023). Canadians generally put the most trust in health experts, including public health officials, local health-care providers, and the World Health Organization. Social media was the least trusted. There was a decline in trust in all eight institutional actors observed in the study by 2022. See figure 5.
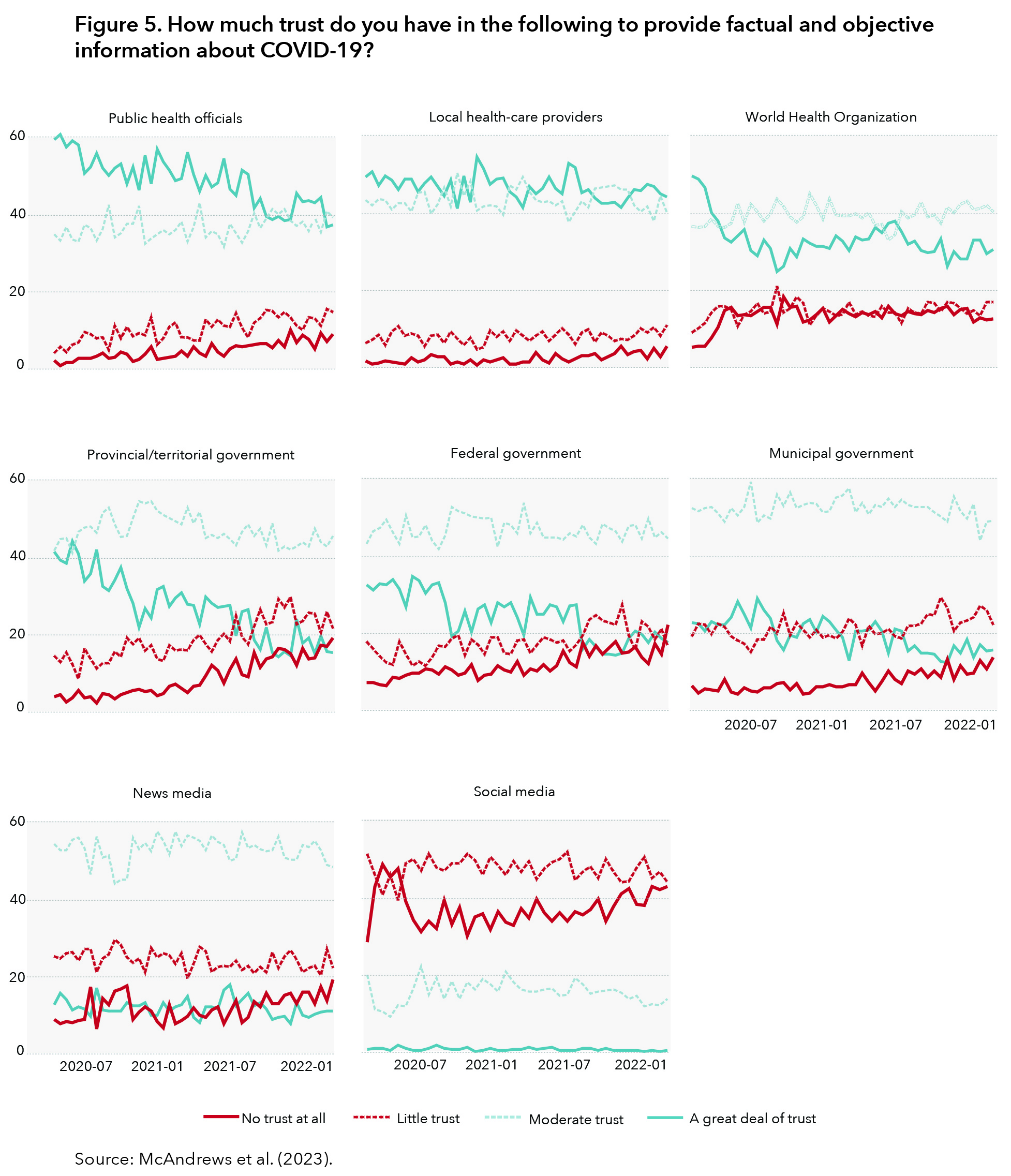
Public institutions gain and lose trust for various reasons. An OECD model sets out five indicators that are thought to influence levels of trust in government: reliability, responsiveness, integrity, openness and fairness. A study by the Institute on Governance examined Canadians’ trust in government using a unique AI model that tracked Twitter data between December 2020 and December 2022. The study found relatively stable average trust in government over the two years but found high variability to specific events. A key finding was that government responsiveness (meaning the extent to which they effectively delivered services and programs) and openness were the most salient of the five components (Institute on Governance, 2023).
Public trust does not exist in isolation. It is formed and informed by multitudes of information sources grafted onto pre-existing biases, perceptions and experiences, both personal and collective. Vaccine hesitancy, for example, was rooted in deeply personal views about science and bodily choice. Opposition to masking and public health restrictions stemmed from world views about personal liberty, community values, religious convictions and government coercion. While the vast majority of Canadians got vaccinated to protect themselves and to help end the pandemic, a sizable minority refused. Paradoxically, it was only when the Omicron variant took hold — infecting even some of those who had been vaccinated — that the divide appeared to lessen. Overall then, the pandemic has had a profound effect on our democratic and public institutions, highlighting enduring challenges concerning trust that persist to the present day.
[1] Primary series means one dose for a one-dose vaccine or two doses completed for a two-dose vaccine.
What We Heard
At the Resilient Institutions conference, academics, public servants, health-care practitioners, politicians and community organizations shared first-person accounts of working on the institutional front lines during the pandemic. The conversations took place under the Chatham House rule, meaning that information about the discussions can be shared but cannot be attributed to any speaker.
The following summarizes what we heard during the event. Each of the eight 90-minute roundtables included four to five speakers. (See Appendix B for the full program.)
The Roundtables
Public Health Decision-making During the Pandemic
This roundtable brought together individuals who played key public health roles. It examined how decisions were made, whether existing governance structures and processes were sufficient and how new ones were adopted. It also discussed what information is required for decision-making in a time of intense uncertainty and how the public should be engaged in these decisions.
A clear view was that the main institutions around public health decision-making within government generally worked as designed, although they were strained. Cabinets — federal and provincial — and supportive governance structures also worked as advertised, being able to make decisions within our system of responsible government. In all instances, however, governance had to adapt and be reconfigured to meet the volume, pace and scope of decision-making that was demanded. This also extended to the intergovernmental infrastructure around health care, such as health ministers’ and deputy ministers’ tables. All of these had to be supported by intense, daily engagement by public servants and ministers.
A key adjustment that governments had to make was to configure their decision-making processes to bring a “whole-of-government” approach in recognition that the pandemic was much more than just a public health issue. It touched the economy, schools and many other areas. There was a clear need for officials to work collaboratively across departments. This type of governance structure had to be put in place in many instances because it did not necessarily exist beforehand. At the federal level, a dedicated COVID-19 cabinet committee was created to co-ordinate the government’s response. Existing federal-provincial-territorial structures (such as the Conference of Deputy Ministers of Health) provided avenues for collaboration while governments at all levels set up various task tables and task forces to support rapid, focused decision-making.
However, institutions by themselves were no guarantee of success. It was necessary to adapt, reconfigure or set aside the usual rules and procedures to get things done quickly and effectively. Fostering strong interpersonal relationships within and across governments was incredibly helpful — a type of collaborative governance. Our permanent institutional structures did not anticipate the magnitude of the pandemic. The country was not prepared with adequate stockpiles (e.g., PPE, medical equipment and supplies, pharmaceuticals). On the other hand, through imagination and commitment, programs were developed and rolled out at an extraordinarily rapid pace.
We heard mixed reviews about the success of Canada’s health-care sector and institutions. Participants noted that Canada’s low mortality rates relative to other countries were likely due to its strict public health measures. That said, Canadian hospitals were already facing a capacity crisis prior to the pandemic and needed to respond in unprecedented ways when faced with a significant increase in new, critically ill patients. Measures such as hospital transfers were implemented to overcome capacity challenges. We also heard about pre-existing cracks in the long-term care systems, which contributed to the devastating outcomes that were experienced. On the scientific and research capacity side, we heard about the extraordinary conversations and information sharing that occurred between scientists and researchers globally. We also heard that the capacity of Canadian scientists to conduct clinical trials, which evaluate the effectiveness of health interventions, was limited by a poor information infrastructure with inadequate real-time access to insights and information.
First Nations communities faced low public health capacity and inadequate disaggregated data, as well as systemic biases that privileged Western conceptions of health and medicine. Some of these factors were overcome by developing culturally sensitive communications and interventions. However, it was noted that work should be done to ensure that governments and officials trust Indigenous communities more to understand and deliver for their membership, as well as have the necessary training and tools. One participant said:
“That capacity has to exist at several levels. . . . The providers who work in the community need more public health training. Education is huge. The middle band of decision-makers, policy analysts, health-care providers and others [need] to really understand because they’re blind [about] . . . how health care works in the First Nations community. It’s not something that people are trained to understand.”
We heard that future pandemic preparedness should determine how best to minimize public health impacts (e.g., morbidity and mortality) while also minimizing social and economic disruption. To achieve this, advisory structures must support integrated and co-ordinated thinking. Public health evidence was a central input for decision-makers during COVID. They also should have considered the broader scientific context as well as societal, economic and community impacts. However, advisory structures did not always enable this type of integrated thinking. It was recommended that models be gleaned from other jurisdictions. One participant reflected:
“I remember more than one cabinet minister saying: ‘Where does the integrated thinking, the integrated advice that brings together all of the considerations [take place]?’”
An additional consideration is the extent to which the advisory function inside governments should retain independence from the decision-making and implementation functions when establishing public health advisory relationships and structures. We heard that the role of independent advisers — who may feed evidence and speak independently about the impact of a policy — is different from the role of government policy implementers. Both need to work together symbiotically, but there also needs to be clarity about the distinction between them.
Participants discussed how challenging it was to share messages about public health decisions and build public trust. Canadians heard from so many different voices and received a huge volume of often complex information. Decision-makers were also dealing with anxiety within certain communities, as well as growing misinformation and disinformation. Embedding a communication specialist within scientific or public health teams was suggested as one means of improving communication with the public.
Data Production and Data Sharing in the Canadian Health-care System
The pandemic highlighted the crucial role that data play in informing health-care decisions and how imperative it is that we improve the sharing and use of data across Canada. This roundtable brought together experts to identify how we can better collaborate on this issue across levels of government. It included policy leaders with insights into Canada’s current challenges surrounding data sharing.
A key message was that Canada’s data collection processes and mechanisms are not equipped for real-time data flow. We heard that improving data flow should be a priority during the development phase of data systems so that structures can be built with this priority in mind, recognizing that it did not happen when these systems were built in the past. One participant characterized the current data structure in Canada as “towns or cities with no highways or infrastructure to connect them.”
This was especially problematic during the pandemic because of issues such as where to distribute vaccines, PPE and health-care human resources. These issues required quick decisions, but leaders did not have access to data to determine where resources were best utilized and to determine the results of diverting resources to certain communities. Panellists noted that Canada’s existing data systems are designed to track long-term changes or review results after a crisis has ended. Additionally, because of the lack of interoperability, spotting patterns in the existing data and forming a real picture of the situation in Canada is challenging. As one participant pointed out, you cannot take proactive actions to address emerging issues if you cannot see that those issues are emerging. The panellists stressed that the cost of not having these real-time data flows must be made clear to Canadians. There is also a lack of capacity to understand data and translate them into useful information, as well as challenging issues with recruiting people to build this capacity.
The panellists proposed several reasons why Canada’s failures in data sharing at all levels of government have endured since SARS, including technological complexities surrounding the infrastructure that exists to share data and the regulatory disentangling that needs to be done. For example, there are no standards surrounding data governance that have been universally accepted. Panellists identified one of the main issues in data sharing as confusion around data privacy legislation or a reluctance to share data that are hidden under the guise of adhering to privacy legislation. Several panellists argued that privacy concerns are largely a red herring and that there are many avenues to ensure there are checks and balances. One noted:
“We cannot have institutions, organizations, levels of government that are using the notion of a data steward to essentially hold data from actually getting to where it needs to [go] so that we can get at the insights in a real-time, consumable fashion.”
Panellists ultimately argued that these constraints would be largely solvable if not for the culture of information guarding and risk aversion that prevents information from getting where it needs to go. For example, there’s a nervousness among provincial governments about possible misuse of the data. One panellist said:
“It’s a real double-edged sword for them. Data can be weaponized [against] them. They’re nervous about this because often it’s used in a politicized way.”
However, the flow of these data is crucial to the flow of benefits. Panellists argued that Canada must ensure those benefits are distributed among different levels of government and stakeholders. The culture of hoarding such information must be changed. One participant suggested an independent body, such as the Canadian Institute for Health Information, could keep track of data gaps in the system, improving transparency around which provinces and territories are sharing data and which are not.
Another aspect of data sharing that panellists noted was disaggregated data. Decision-makers need to understand which socio-economic characteristics impact a successful outcome and identify patterns to adjust policies accordingly. Panellists challenged the idea that the current system of data serves everyone equitably or fairly. They noted that holding onto this notion can contribute to gaps in our system. The expertise necessary to challenge enduring inequities does not exist internally. Questions arise in communities that have been harmed by governments in the past about how to build trust. Trust is needed to obtain data from individuals on elements such as race, occupation, postal code, education, etc. Disaggregated data are essential because they can reveal how crises have impacted their health and socio-economic outcomes.
One panellist mentioned that the push for disaggregated data came from Black and Indigenous communities that understand the importance of being able to measure outcomes. Good data governance can be a mechanism to build trusting relationships with people who have been systematically disenfranchised, thus ensuring their participation, as well as transparency and accountability. An example of trust-oriented data collection could be the recognition of the unique constitutional status of First Nations, Métis and Inuit people, and the acknowledgment of Indigenous data sovereignty rights and principles through bilateral information-sharing agreements at both local and national levels.
Intergovernmental Relations During the Pandemic
The pandemic marked one of the most intense periods of intergovernmental relations in Canada’s history. This roundtable sought to provide a deeper understanding of the challenges and opportunities in this area in times of crisis. In addition, the panel considered how Canadian governments can implement those aspects of intergovernmental relations that worked well during COVID to improve our response to future crises. This roundtable included policy leaders with insights into the evolution and state of intergovernmental relationships during the pandemic.
There were diverse views on whether intergovernmental relations facilitated or inhibited the pandemic response. Most panellists agreed that the degree of communication between the different levels of government was high when the coronavirus first emerged. However, a key insight we heard was that, after the initial period of togetherness, there was significant variance in the amount of communication, and consequently the degree of co-ordination, between different levels of government.
We heard that relationships between some municipal governments and their provincial counterparts were frustrating, with municipalities expected to implement many provincial programs with little direction or notice from the province. Municipalities also faced significant revenue reductions and consequently had to lay off public servants despite having an elevated workload. Because information exchanges did not happen consistently between municipalities and the provinces, many municipalities turned to each other, both domestically and internationally, using established forums to facilitate information exchange that shaped their policy response. One participant gave a surprising insight into how minimal the dialogue really was by noting that one premier communicated with that province’s big city mayor only once throughout the entire pandemic. Another viewpoint raised by panellists was that a certain level of friction was to be expected, given that all levels of government were in crisis mode. Therefore, the exclusion of some governments from certain conversations may not have been intentional, but rather done out of a desire to get policy out the door quickly. One participant noted:
“When I was talking to some colleagues, it really felt that we were cut out even though we were delivering all the services on the ground.”
Similarly, Indigenous leaders trying to secure PPE and vaccines for their communities were frustrated by poor information sharing from other levels of government. However, once the dialogue began, Indigenous leaders were able to relay their policy solutions and logistical plans. They just needed a partner at the decision-making table to facilitate the implementation of those plans. This experience communicated a key lesson: that the exclusion of Indigenous leaders from the decision-making process during COVID was a product of a relationship allowed to erode over centuries. It is paramount to build that relationship on an ongoing basis. Panellists heard that in future emergency management planning, Canada must be more inclusive from the start on the role of Indigenous leadership and governments.
The experience of both municipal governments and Indigenous governments was indicative of tensions surrounding the question of jurisdiction, such as: Who does what? Who pays for what? One panellist mentioned the stark difference between cities that were “bleeding money” and provincial governments announcing surplus budgets, as well as the resentment that was thus created. Provinces and territories faced similar tension with the federal government because many costly services such as health care and infrastructure are largely the responsibility of the provinces, which have less ability to generate revenue than the federal government.
There were some triumphs. The federal government was very proactive at reaching out to large municipal governments and fought to bring provinces to the table when necessary. It was also more willing than usual to leave rules, practices, jurisdictions and procedures at the door and orient itself into a configuration best equipped to address the issue at hand. A shared goal across actors was a powerful avenue for breaking down institutional hurdles to collaboration. One participant noted that there were weekly first ministers’ meetings throughout a significant part of the pandemic, which was unprecedented.
At first, provincial and territorial governments reached out to each other for information sharing and exchanging best practices, but this communication diminished after the initial crisis phase had passed. There was little incentive on everyone’s part to maintain these relationships. One participant noted that the return to pre-pandemic levels of communication was not cause for concern because maintaining these crisis-phase relationships is resource-intensive and those resources can be better delegated elsewhere when not in an emergency. The challenge is figuring out what COVID-era processes should become permanent and what can be retired. There may be an instinct to retreat into pre-COVID practices, but governments need to review systems and see what should be preserved. A good start would be to look back at decision-making processes and see how agility can be improved in the long term. One participant said:
“There are improvements that can be made. I think the instinct is to kind of retreat back post-crisis into regular operations. Frankly, when people are exhausted, they kind of feel: ‘Ok, now I can sort of get back to my regular thing.’ [Instead] we’ve got to actually think about a systems review . . . to be able to take those lessons learned.”
A final point of discussion was whether we need new institutions or to keep existing institutions working as they should. One panellist proposed the revival of a federal minister of state for urban affairs to rectify some of the isolation that municipalities felt during the pandemic. Other panellists felt that it would be better to focus efforts on bringing municipalities and Indigenous governments to the intergovernmental forums that already exist. They argued the system would be better served by improvements to its existing structure, rather than the creation of something different.
Imagining a Federal Community That Works
The pandemic highlighted the strengths and weaknesses of Canada’s federation. This roundtable brought together senior civil servants, elected officials and private-sector representatives to consider how better co-ordination and collaboration could be built across all orders of government for a more resilient federation.
The roundtable ruminated on the future of the federal community — one that doesn’t include just the federal, provincial and territorial governments, but also Indigenous governance structures, municipal governments, non-governmental organizations and the private sector, etc. This discussion could be viewed as a continuation of the previous roundtable on intergovernmental relations.
Jurisdiction was a core facet of the narrative of the pandemic. In the beginning, governments were able to “get out of [their] own way” and put traditional jurisdictional squabbles aside to move faster and deliver in a way that was starkly different from the historic norm. Due to the way the pandemic affected all aspects of government, many policy leaders found themselves forming relatively new relationships and building trust quickly. But the traditional squabbles could not be delayed forever when the galvanizing, common objective had been met, particularly when it came to the way the federal government exercises its spending power. For example, as part of the federal safe restart agreement, education funding was made available to provinces and territories. However, it was made available with strings that some provinces viewed as infringing on their exclusive jurisdiction in this area.
We also heard that, outside these jurisdictional tensions, Canada needs to consider why the conversation around a federal community ends with just federal, provincial and territorial governments. Other actors such as municipal and Indigenous governments could have had a positive impact on outcomes and it was a bad choice to exclude them. We heard that we need to have a conversation about what the new baseline of intergovernmental relations should be going forward to set up the country for growth, competitiveness and success.
In light of these evolving tensions, a core question at this roundtable was whether we need new institutions to adapt to new challenges or whether existing institutions are sufficiently able to handle the increased pressures that emerging crises exert. Panellists were fairly divided on this question. Participants identified that a clear first step toward answering this question is to determine how agile our institutions were during the pandemic.
Some participants thought Canada’s COVID-19 response demonstrated the flexibility of our institutions because there were several reports that governments were willing to “leave jurisdiction at the door” and get results. The pandemic response didn’t require governments to rewrite laws or make changes to the institutional landscape to facilitate this. Participants posited that what we saw during the pandemic was a solid system on steroids, with capacity ratcheted up but on a firm foundation.
However, some participants viewed the pandemic response as placing too much of a burden on public servants. They argued that while Canada was able to do things differently, these were workarounds and not long-term sustainable changes. We heard that Canada needs to have a conversation on how to transition workarounds into long-term, bolder, forward-thinking options to improve its global competitive edge. Panellists observed that governments were returning to processes in place before the pandemic and cautioned against losing the opportunity to retain some of the flexibility that emerged from the pandemic response. As one said:
“The system had worked for many years but, during the pandemic, it had to go on steroids. We had daily calls with IGR [intergovernmental relations] counterparts across the country. We had first ministers’ meetings every week instead of once a year . . . but you don’t need to sustain that level of engagement post-pandemic.”
Moreover, panellists thought the institutions we have do not work toward Indigenous self-determination. While governments did improve, relative to prior emergencies, on incorporating Indigenous participation and dialogue into their COVID-19 response, there is a worry that in the aftermath, the momentum for the true implementation of Indigenous self-determination will disappear. Panellists suggested there need to be incremental changes toward placing confidence in Indigenous Peoples, institutions and leadership to make decisions about Indigenous destiny — and that may lead eventually to creating new institutions.
Panellists also discussed factors that could stunt the evolution of the federation. A potential barrier to these transformations is the fractured relationships between different orders of government during COVID-19. Some participants mentioned that the propensity to trust and collaborate between governments is not as strong as it was before the pandemic because of competition for resources such as PPE and vaccines, as well as general disagreements about pandemic approaches.
The federation will have to navigate the economic shock and the uncertainty that the pandemic caused, on top of the existing long-term economic issues the country grappled with prior to it. From a fiscal perspective, the crisis is not over and the situation has become difficult for public finances. A complication within a complication is that the fiscal imbalance between different orders of government looks very different after the pandemic and this can impact how governments approach policy negotiations, especially from a federal perspective. This will change the way the different governments approach relationships with each other. These factors taken together could mean some friction as governments try to convert pandemic lessons into long-term changes. One participant concluded:
“It’s important to acknowledge, while we were able to do many things differently — and that was a good thing during the pandemic — the reality is that those were workarounds. We were able to do good things in spite of the status quo, not because of it. So can we continue to ride that train into the future? I hope we don’t.“
Public Service Delivery and Governance
This roundtable featured experienced public-sector practitioners and thinkers reflecting on the institution of the public service, its governance and service delivery during the pandemic. They discussed how the delivery of public services adapted and changed in response to the exceptional circumstances presented by COVID.
The pandemic moment was unique in that governments were almost singularly focused on one issue and there were essentially unlimited resources to deal with it. Some participants cautioned against assuming this experience could be adopted as a way of doing business across public services as a whole. “Incident response” is not typical governing. Many day-to-day government activities and operations proceeded without interruption, out of the public eye and were taken for granted. At the same time, governments had to reconsider the reach and scope of their responses. Decisions in one area cascaded to affect others. For example, ensuring that health-care workers were able to staff hospitals became problematic when child-care centres were closed and those health-care workers had to stay at home with their children.
Public-sector workforce characteristics that were important for success included the ability to collaborate, use technology effectively, triage and act with empathy. This was common to both federal and provincial governments. A key message was that, while government institutions were generally successful in achieving outcomes for Canadians, the pandemic experience demonstrated that public-sector institutions and systems — particularly data and IT systems — are not set up for resilience. Success often entailed working around existing systems and required a great human resource investment and cost. One participant summarized it this way:
“I think at a performance level in terms of Canadians getting the support they needed in the crisis, the outcomes were excellent. But heroism is not a great strategy for a systemically resilient institution.”
We heard about the need to invest better in the fundamentals. In particular, the pandemic showed that the hardwiring in the public service — including HR, procurement, pay, and IT processes and systems — needs to be revamped. These internal aspects do not always receive adequate attention until they are broken, but they are slowing down the public sector and could be key to equipping governments for future success. The pandemic demonstrated the importance of investing in training and technology redevelopment — both of which are essential to the long-term success of our public institutions but both of which are easy targets for politicians seeking budget cuts.

Participants spoke about the need to develop government policies and programs in normal times with a bias toward simplicity and using modern IT platforms, so they can more readily scale and adapt and be tested in real time. Policy complexity can build rigidity into policy implementation, which can be particularly hard to overcome in a crisis. Illustrative of the need for simplicity and effective technology was the case of the development of the Canada emergency response benefit (CERB). While the government was able to rapidly develop and deploy CERB, the complexity of the existing employment insurance (EI) system and the outdated IT platform it used made this an immense challenge that required technical workarounds and “heroic” efforts by public servants. We heard from one participant:
“If we cannot come out of this crisis having fundamentally transformed the backbone systems, we’re not going to be able to really leverage the many innovations and we will have wasted the crisis.”
We also heard about key ways the public sector adapted to react responsively and rapidly. Risk was viewed and managed differently. Therefore, there is a window of opportunity now to think about how risk management in the public sector can be optimally approached to facilitate innovation and rapid service delivery while also maintaining accountability. The relationship between public servants and elected officials became more fluid than in pre-crisis times. There was more open communication about errors and course direction, which were almost inevitable given the rapid rollout of programs and policies. There is an opportunity to continue fostering this type of honest dialogue and for the public service to reinvigorate its “speaking truth to power” function. One participant noted:
“We were in ministers’ offices instantly to talk about what the problems were and how to find a solution. This is a superpower that we could be using all the time . . . that honest, transparent exchange of information to make sure that nobody is surprised.”
Lastly, we heard about the ways that different types of departments and all orders of government were heavily involved in the lives of Canadians. Provincial and territorial governments, as the order of government responsible for more direct services, had a different relationship with citizens than the federal government and were often tasked with communicating information that had particularly concrete ramifications for Canadians, such as school closures or policies around hospital visits.
Public Servants’ Roles and Skills for Tomorrow
This roundtable considered the future of the public service post-pandemic from the perspective of public servants’ roles and skills. It discussed what the public service of tomorrow should look like and how it can become more agile, adaptable and digitally focused.
Frank discussion took place around public service quality and effectiveness because any conversation on post-pandemic skills for public servants could not be divorced from the current public service systems in which they work. As in the previous roundtable, we heard that our public service institutions and public servants faced incredible demands to deliver new programs and services under intense time constraints. In many cases, outdated IT and data systems and processes were pushed to the brink of collapse. A prevailing sentiment was that Canada got through the pandemic in spite of these systems. One participant said:
“I think number one, Canada got through COVID, on the federal side, at least, not because of our systems, but in spite of our systems. … Most departments spent the first couple of weeks if not the first couple of months, not fighting COVID. They spent the first couple of weeks and the first couple of months fixing their organizations.”
The pandemic exacerbated an already strained public service in many respects. All participants, however, noted the exceptional work of public servants in rising to the COVID challenge. On the sustainability of this, one participant said:
“So if I had kind of one wish, I would want it to be that the public service starts to become boringly excellent, rather than sporadically heroic.”
Chronic issues — well known inside and outside the public service — include burdensome hierarchies, slow approval processes, risk aversion, outdated HR processes and siloed structures. These issues will stifle innovation in normal times. One participant put it this way:
“Much of the discussion around Canadian public administration is a bit of a broken record, to be honest. You can find the clerk’s reports from decades ago; you can find academic analyses from 30 years ago; you can even go back to the Glassco Commission in 1960. [You will] see people commenting on the sclerotic, excessively burdensome, top-down hierarchical approval processes, limited scope for collaboration, a deep risk aversion and fear of public-facing failure that makes it difficult to be creative and innovative.”
Compounding chronic public-sector challenges is the fact that Canada is increasingly operating in a rapidly evolving, complex and even dangerous world characterized by emerging threats. It may be impossible to anticipate specifically what kind of crisis will come next, but building systems that work will best set up the public sector to succeed. One participant reflected:
“The world outside us is changing rapidly. The world outside us is getting more dangerous. The world outside us is getting more hostile. I’m not sure that our institutions [are] equipped to face the emerging realities that Canada will be going through.”
Common to solutions-oriented discussions during this roundtable was the view that courageous and empowered leadership is needed to take on issues within systems that are highly averse to risk and change. We heard that leadership, especially at the executive level, and incentivization to encourage risk-taking are needed both to address long-standing backend issues, such as outdated HR and IT processes, and to make lasting cultural changes that will enable continued modernization of the public service. Dynamic people need to be in these roles that address complex policy issues. Citizen pressure for improved service delivery could equally be a catalyst for public-sector reform.
We also heard about a skills crisis that impacts Canadian governments. The public service needs to anticipate more proactively what skills will be needed in the future, build and transfer these skills, and create work environments that retain talented employees. All the while, key public service values, such as impartiality and commitment to service, should remain the bedrock. Canadians are highly educated and trained but there can be a mismatch between the skills that people have and those that are in high demand in the contemporary workforce. One participant recognized the acute talent shortage but also noted that there is an existing pool of talent within the federal government that has not been tapped because executives in particular have “not been asked to consider what a modern service organization should look like.”
What skills do public servants need now and in the future? Participants highlighted soft skills such as leadership, resilience, stamina, entrepreneurialism and good judgment as essential during the pandemic and important for the future. One participant suggested that skills that need to be built include digital literacy, an understanding of responsible AI safeguards and stakeholder management skills. While some groups in government are strong at stakeholder engagement, there was a recognition that more can be done to ensure stakeholders and citizens are meaningfully engaged in the design and development of policies and services. One participant asked:
“How does that meaningful input come in a way that’s not tokenism in terms of how you’re talking to Canadians?”
The increasing use of artificial intelligence (AI) and other disruptive technologies will also have a significant impact on the future of work. The public sector has an opportunity to be proactive about how it leverages these technologies, while also ensuring responsible management and use.
The pandemic and onset of remote work supercharged innovation in the public sector, including in digital government. Fundamentally, the pandemic required governments to re-examine the “web of rules” around service delivery and program development. However, there is concern that the momentum of digital innovation in government is slowing now, given that many of the structural realities — for instance, hierarchies, slow approval processes and siloed structures — remain largely unchanged from the pre-pandemic period. Participants noted that lasting advances will require strong leadership, structural changes and new incentives. We heard about missed opportunities to make long-term policy or legislative changes based on short-term adaptations from the pandemic period. According to one participant:
“It’s an uphill battle to be innovative in the federal public service. There are so many rules and procedures, rules and processes that make it overwhelming … That is a really common narrative in our federal public service right now.”
Participants discussed issues of equity, diversity and inclusion (EDI) in the public service. We heard that leaders need to be held accountable for results in this area and that EDI work should not be limited to hiring practices but should also be about building an inclusive culture. A representative public service requires a representative executive cadre.
The Public’s Experience of Dealing with Institutions During COVID-19
This roundtable focused on the views and experiences of the broader population beyond government. It examined how institutions performed during the pandemic from the public’s perspective and suggested that diverse voices not be overlooked in future crises to make for a more inclusive decision-making process. This roundtable included policy leaders who represented different civil society/community groups, who shared their experiences interacting with governments during the pandemic. A key theme that emerged from this conversation was trust.
Participants emphasized the need for governments to build trust within different communities, but also for governments to trust the expertise and knowledge of community leaders and equip them with resources and decision-making power. Some participants expressed frustration that, although community leaders did a lot of work to get buy-in from their respective communities, they also had to fight for seats at the decision-making tables. That meant the loss of precious time that could have been used to improve certain policy outcomes (e.g., vaccine distribution). One participant remarked that there is no alternative to the relationships that community leaders build with their communities and that governments should include these leaders from the start in the next crisis.
Another complication we heard was that jurisdictional wrangling made it difficult for these leaders to identify where to receive support for their communities. Participants noted it was particularly difficult to get material support from the provinces while federal officials were difficult to reach directly. Indigenous groups were neglected by different orders of government because of confusion surrounding which was responsible for giving Indigenous communities economic and public health support. Indigenous Peoples living off reserve were often overlooked for pandemic support and any resources that were allocated to them often did not address priority needs. All community organizations spent significant time and resources pushing governments to adjust how support was delivered. If community groups had been involved from the beginning, policy delivery would have been better. One participant noted:
“The problem was that the provinces weren’t showing up. I had one guy from the federal government [involved] because they’d already been on another call with Indigenous representatives. So it was a challenge to try to get . . . the provinces and the feds coming together. They wouldn’t come to the urban table. So, it was just urban Indigenous organizations talking to themselves about how to meet this great need — with the one guy that was assigned to be on those calls. He was great. He did everything that he could and he did help move things along. But that was definitely a challenge.”
We also heard that trust in institutions was high at the beginning but significantly decreased over the course of the pandemic. Political affiliation is an unavoidable piece of context when it comes to trust. People’s trust in government tends to increase or decrease depending on whether their preferred political party is in power. At the beginning of the pandemic, leaders across different political parties were united on COVID-19 messaging, which helped with public support. But as that unity waned, so did public support for pandemic measures. Public trust also fell along party lines — whether the public felt that they were represented in their government or not. The public also lost trust in institutions when there was perceived policy incoherence. For example, one participant remarked that, when community members felt that policy unfairly impacted certain groups, their willingness to comply with pandemic measures declined. Another participant recommended that governments need to review pandemic measures and weigh the societal and personal costs to minimize disruptiveness to people’s livelihoods.

One exception to the decline in trust was public health workers (e.g., doctors, nurses and other health-care practitioners). Surveys revealed that trust in this group remained steady throughout the pandemic. However, there were complications in this regard too, especially pertaining to vaccine rollout. For example, ethnic minorities were often unable to get instruction in their language on health orders and therefore found it hard to comply with them or were forced to do the translation themselves. Participants recommended that governments identify where different demographic groups get their information (e.g., through WhatsApp channels, ethnic media, word of mouth, religious organizations, etc.) and meet the community where they were. One participant noted:
“They weren’t connecting with the community. They didn’t know what the needs of the community were … [The community was] not watching mainstream media. They were actually watching ethnic media … It was incredible to see that trust develop by leveraging ethnic media, which many institutions didn’t know how to do.”
Trust, Communication and Decision-Making
This roundtable consisted of elected officials, commentators and academics who reflected on how our democratic institutions performed during the pandemic, focusing on public trust and communications. It discussed ways to foster a stronger relationship between elected officials, governments and citizens in the future.
The pandemic challenged governments and leaders to find effective ways to communicate clearly, rapidly and frequently with Canadians on a virus over which they had little control, with often incomplete, confusing and changing information on the science and data behind it. Because of this, evidence-based communication was difficult as the pandemic wore on. Public trust was inevitably affected.
This was to be expected, both because information was rapidly evolving and because citizens needed real-time information to make decisions that affected their health, daily activities and livelihoods. Governments adapted how they communicated. For instance, the federal government set up an integrated communications team to maximize outreach and manage the volume of outreach, recognized the need to tailor messages to different communities, and increasingly used behavioural science to better adapt communications with citizens.
Animating the roundtable was a view that a distinct division can be observed between the pre-vaccine and post-vaccine phases of the pandemic. At the beginning, there was a sense of unity around “flattening the curve,” as well as visible collaboration across party lines and between orders of government. As expected in a time of uncertainty and crisis, there was also high public trust. This unity was notably fractured when governments began competing with one another for vaccine procurement and when the population became divided, according to their willingness to get the vaccine and then later over their vaccine status.
Political and societal polarization is now being felt profoundly at all levels of political discourse. Participants spoke about a lack of empathy for the vaccine-hesitant and suggested that this in part has contributed to fuelling “seeds of disengagement and marginalization” that are still being felt strongly today. Another societal division stemmed from different experiences of the pandemic, often along socio-economic lines. For instance, office workers who were able to work from home had vastly different experiences than essential workers and those working in service sectors. Today, polarized public debate is endemic at all levels of discourse and there appears to be less civility and ability to find agreement. One participant described the polarization being felt today this way:
“We are pulled further apart than I feel like we’ve been in a really long time. It’s something that is now permeating not just federal politics, but every level of political discourse from the school board election, all the way up. So this isn’t something that a change in one party’s leadership is going to change. This is like a wholesale endemic thing. I don’t know how you get it out of the DNA of our politics now.”
The complexity of communicating during a crisis also contributed to fractured trust in institutions. The absence of a single voice on issues, the changing nature of advice and the prominence of social media created space for doubt and misinformation to thrive. We heard that jurisdictional differences eventually led to confusion and doubt. For example, we heard provincial and territorial medical officers of health communicating different messages than the federal chief medical officer of health. This was sometimes exploited by actors spreading misinformation and disinformation to decrease trust in government messaging. One participant suggested that, as a federation, Canada needs to conceive better approaches to communication that build and maintain a strong, shared public narrative. A possible approach during the pandemic would have been to create a COVID crisis cabinet committee that included members of the Official Opposition and other parties. One participant spoke about addressing the complex communication environment by building more capacity for understanding uncertainty and change:
“A lesson learned . . . [is] how we provide the information, while also reassuring people, but leaving the space for people to recognize and accept that there is going to be change.”
A resounding takeaway was that Canada would struggle to achieve the same degree of initial public adherence to government restrictions in a future crisis. Trust in government, trust in public health and societal trust in one another have all been impacted. At the same time, the pandemic unfolded within an existing democratic and political environment, where political rhetoric is highly polarizing and where many Canadians do not feel that the major political parties understand, or speak to, their realities. One participant noted:
“If your democracy is working really well, there is a synergy between what we say in the House of Commons, what we hear in terms of political rhetoric and what is felt in the public… There is responsiveness; there is a connection. If it’s not working right, then it means there’s some kind of strange, exploitative relationship between political leaders and rhetoric on the one hand and then what’s being felt in the public. There’s a reason why many people are saying they’re politically orphaned.”
Changes to democratic governance, including revisiting the electoral system, political party leadership election rules and campaign finance laws, could contribute to rebuilding a vibrant democracy.
Summing Up: How Did Institutions Fare?
The main goal of the Resilient Institutions conference was to understand how Canada’s public institutions fared during the pandemic and learn from those experiences.
Our roundtable discussions reveal a mixed answer to this question of how Canada’s institutions performed but we can identify three broad perspectives:
- Canada’s institutions performed well, responding ably and agilely to an unprecedented situation.
- Canada’s institutions performed adequately with gaps and weaknesses that needed to be filled at the community level.
- Canada’s institutions performed poorly with inadequate and wrong responses that affected Canadians and reduced public trust.
The conference consensus was clear: Our institutions did not succeed completely, nor did they completely fail. The pandemic demonstrated how our institutions can be agile and nimble, but it also exposed some serious institutional and governance weaknesses that affected government responses and public health outcomes. Those weaknesses need to be addressed. While it is perhaps unsurprising that we heard a mixed review, the nuanced view that emerged on Canada’s institutional success is important for decision-makers to consider. Importantly, these three overarching perspectives are not mutually exclusive. Some institutions were described in successful terms at one moment during the pandemic and in less successful terms at another (see figure 6).
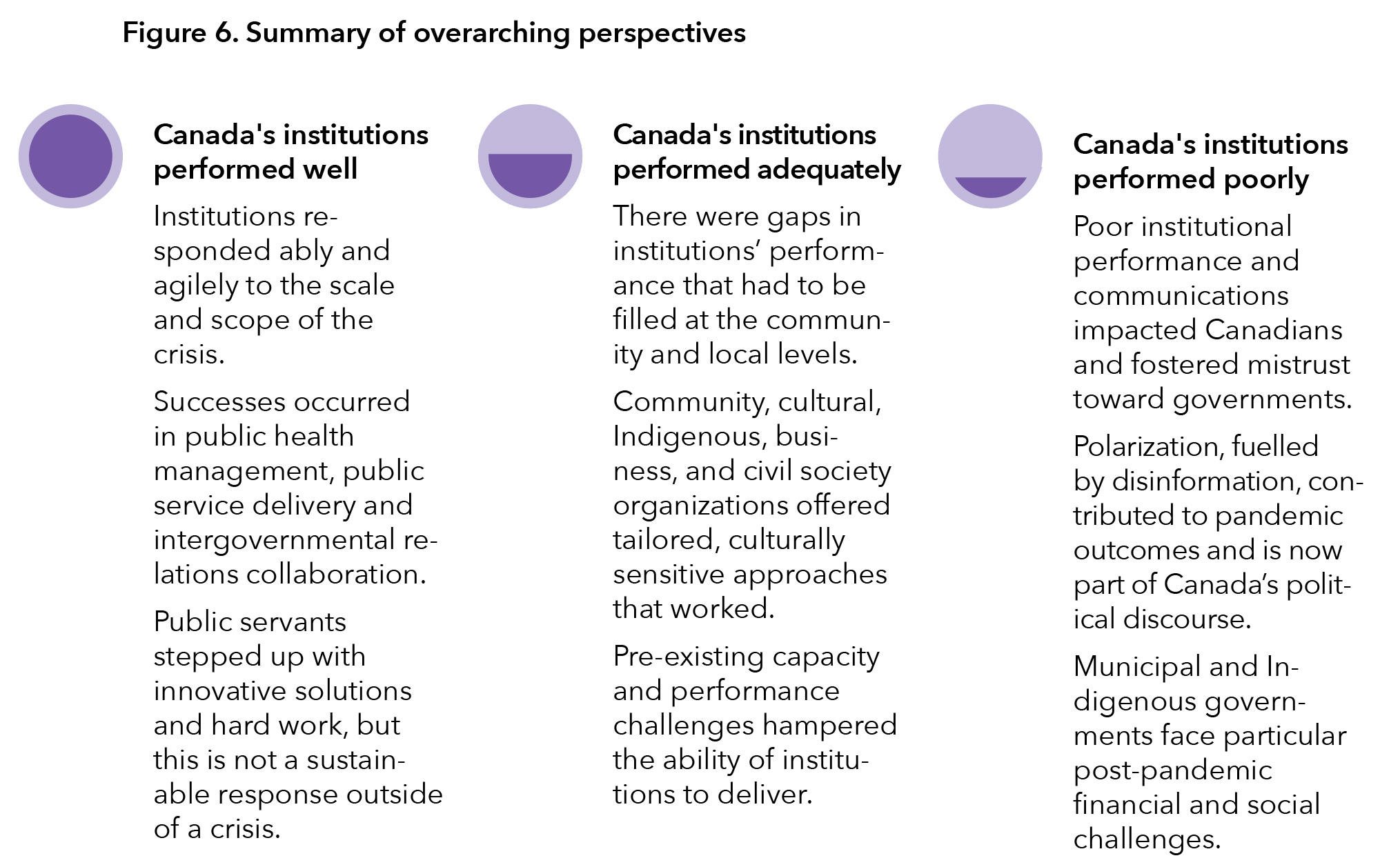
Each perspective offers a key takeaway. Proponents of the first perspective say the pandemic forced public institutions to become more adaptable, which then revealed their underlying strengths. The key is to harness the strengths observed in public institutions during COVID-19 and determine how they can be fostered in ordinary times. In particular, Canada needs public institutions that are more innovative, bold and able to take on complex challenges. Proponents of the second perspective underscore that Canada’s public institutions should invest time and resources to address capacity gaps, design optimal systems and build a strong public-sector workforce both to succeed in normal times and to respond to a future crisis. Proponents of the third perspective highlight how the pandemic revealed and worsened serious issues of trust, polarization and misinformation, and has caused deterioration in some relationships in the federation. They believe that addressing these challenges must be part of any proposal to make our public institutions more resilient.
Perspective One: Canada’s Institutions Performed Well
This first perspective was that, when faced with tremendous stress, Canada’s public institutions generally performed well. The key to this success was adaptability and the capacity to work innovatively within systems and structures.
We heard about how Canada’s system of government was able to adapt to keep operating through unprecedented remote-work directives, while pivoting to confront the pandemic. The federal government was able to develop and deliver large-scale support programs and services for Canadians, such as the CERB, even while much of the public-sector workforce was working remotely and dealing with pandemic restrictions and pressures like all Canadians. Provincial governments provided supplemental and, in many instances, co-ordinated support. A key reason for this was the extraordinary hard work, commitment and innovation of public servants at all levels.
For all governments, public health measures were implemented quickly and relatively effectively in the first instance, which helped the country manage the onset of COVID-19. Canada’s vaccination program in 2021-22 was particularly successful. Public health co-operation and co-ordination across governments was particularly strong. Indeed, intergovernmental relations were in many ways more successful during the crisis than in ordinary times. This success can be attributed to a clear common goal, frequent communication and a willingness to set aside traditional patterns of behaviour.
At the same time, we heard that these institutional successes are neither sustainable, due to the tremendous stress that they put on the public-sector workforce, nor replicable in the absence of crisis conditions. For instance, the daily pace of intergovernmental relations communications is not sustainable on an ongoing basis, nor will there be the same willingness to spend money and direct resources of this magnitude in normal times. As one participant put it:
“Applying the lessons of 2020 is not as easy as one might think. Governments were operating during the pandemic in extraordinary times of collaboration, [with] almost endless resources. Now we are returning to regular governing.”
Perspective Two: Canada’s Institutions Performed Adequately
The second perspective was that the country was generally able to achieve desired outcomes for Canadians and that public institutions performed adequately. However, these outcomes were sometimes accomplished outside — or despite — these same public institutions.
We heard from community, local, cultural, Indigenous and other stakeholder groups about the challenges they faced to be meaningfully included in decision-making. Then, we heard about the successes they had in reaching Canadians through tailored and culturally sensitive approaches — strongly suggesting that this should be normalized.
Several roundtables discussed how community-based strategies were leveraged to increase vaccine uptake. Individuals and community groups stepped up to develop and share information on vaccines and pandemic hygiene in different languages and using culturally relevant approaches. At the same time, we heard that Indigenous, cultural and community groups could have been more involved in formal advisory tables, which would have allowed them to provide decision-makers with the on-the-ground knowledge required to respond best to their particular needs. As a result, many communities, including urban Indigenous Peoples and the unhoused, fell through the cracks and faced disproportionately harmful impacts. Advocacy and community groups spoke about how they needed to fight to get a seat at the table. We also heard about the need in future crises for advice structures that incorporate perspectives beyond public health, such as on the economy, education and social services.
Public institutions also entered the pandemic with pre-existing capacity gaps and long-standing challenges, including outdated government data and IT systems and processes. Health-care systems were already operating under strained circumstances pre-pandemic, with significant human resources constraints, along with data-sharing platforms that were not optimally set up for a crisis. These existing challenges were amplified by the demands of the pandemic, which resulted in cancelling and delaying health-care procedures. That backlog is still with us today.
Perspective Three: Canada’s Institutions Performed Poorly
The third perspective is that Canada’s public institutions performed poorly during the pandemic and we now face heightened issues due to fractured public trust and fragmented social cohesion.
Trust in institutions was a key theme that emerged at the conference. We heard that the pandemic impacted trust in our institutions generally and trust in public health institutions and public health officials more particularly. This can be attributed to numerous factors beginning with the long, grinding duration and scope of the pandemic. Perceived policy incoherence and the blunt nature of certain public health measures contributed to widespread pandemic fatigue. That was exacerbated by shifting scientific evidence and advice about how to respond to the virus itself, by jurisdictional differences in approach and by inconsistent communication from public officials. Social media provided an effective channel for misinformation and disinformation actors to operate.
Thought leaders from Indigenous communities identified structural racism and discrimination within public institutions that continue to critically impact trust in institutions and the health-care system. One participant bluntly noted:
“The system is intrinsically racist. Because of that history, that constant facing of structural racism in the system, there is no trust.”
We also heard about fractured relationships between Canadians which developed in part from different experiences of the pandemic and diverging views on public health measures – both of which were worsened by polarizing political debate. The Ottawa truckers’ convoy episode in January-February 2023 and barricades at U.S. border crossings in Alberta and Ontario were the most significant manifestations of that polarization.
The pandemic shed light on, and worsened, certain relationships in the federation. The early positive tone of first ministers ultimately gave way to more typical arguments and recriminations. We heard about strains on the provincial-municipal relationship, as well as huge financial deficits faced by municipalities that are now on the frontlines of addressing other crises, such as housing and toxic drugs. There was also recognition that the health-care system does not serve everyone equitably and that this contributes to the health gaps that were experienced during the pandemic. One participant concluded:
“Your postal code mattered. Your ability to survive, or not get the kind of help that you wanted, was very dependent on where you lived, the kind of job you did and the exposure that you had. Your race was a huge determinant. The type of housing and how many people [lived in one unit or house] all had impacts.”
All of these issues now form part of the post-pandemic Canadian agenda for governments.
What Worked, What Didn’t and What to Do About It
Part II of the report highlighted what we heard during the conference and summarized each roundtable, concluding with the participants’ evaluation of how the four institutions performed during the pandemic. These participants — public servants, decision-makers, community leaders and public policy specialists — had all been in the middle of Canada’s pandemic response.
Part III consists of our conclusions and recommendations based on what we heard, considered and then examined through subsequent research. Four key lessons capture the most significant learnings. We then set out 12 specific recommendations — three for each lesson.
These recommendations are addressed principally to governments and by extension to all Canadians. They also touch upon civil society organizations and public policy stakeholders. Each recommendation is part of what we believe the country needs to do to ensure that Canada learns real lessons and acts to make our institutions more resilient to help us react to future crises.
Our goal has always been a positive one — to learn and change, not blame and shame. It is not meant to identify any failures of specific politicians or public servants but rather to assess institutional performance. We seek to be better equipped to fight the next battle, not relive the previous one. Like all Canadians, we are looking forward.

If there is one overall conclusion we can draw from how the country responded to the COVID-19 pandemic, it is that people step up in crises. For the most part, Canadians came together, at least at the beginning. But this is no substitute for having the institutional capacity for governments to respond actively and properly. You cannot build resilient institutions solely around the dedication and professional heroism of public servants and community leaders. Governments have grown in size over the decades; however, they have done so with insufficient regard for the underlying institutional infrastructure of people, systems and processes that govern performance.
The pandemic taught us that institutional capacity cannot be taken for granted. It was not always present, adequate, monitored or measured. It was not aligned in key areas — such as data and IT systems — to support what governments needed.
In a time of expected funding restraint for governments, a core priority should be placed on ensuring essential institutional capacity is present, up to date and ready for the next crisis.
Recommendation 1: Retool and reinvest in the public service’s digital and IT infrastructure
The slow hollowing out of the fundamentals of the public service — human resources, IT infrastructure, training and procurement policies — inhibits its capacity to respond well in a manner that is both innovative and accountable. If we want our institutions to be resilient, we need to invest in their foundations.
Several panellists pointed to how the public service does not have the internal capacity to carry out key work and depends on external consultants to fill these gaps. In addition, many of the actual physical systems used by the public service are at the end of their useful life. In the Part II roundtable summaries, we gave the example of the systems on which employment insurance runs.
Renewed investment in these systems is needed. As we enter into a period of budgetary restraint and new fiscal choices, there is every prospect of this being postponed. Politically, these are never attractive spending choices. Investing in internal government operations does not win votes come election time. But doing so is essential for good service delivery of programs and making internal government processes more efficient and productive — something citizens do appreciate. Responding to the next crisis will be made easier if we know that the systems needed to do so were built for the century ahead, not the one behind.
Therefore, governments must invest in the physical and technological infrastructure of the public service. At the same time, simply pouring money into IT systems is not enough; the way they are managed and rolled out must also be rethought.
Updating and transforming long-standing systems and processes will not be an easy task, but many solutions have been repeatedly identified by internal and external voices with no significant follow-up. As former federal public servant Sean Boots told the 2023 FWD50 conference, simply making incremental changes — rather than more courageous, revolutionary change — has caused Canada to fall behind other countries in public service delivery. “Here in Canada, our processes and organizational culture put up a bunch of barriers to doing things differently, and the established status quo processes keep on failing over and over again,” Boots noted (Boots, 2023).
A strong and shared commitment at the political and senior officials’ level is required to take on these systemic challenges. To kick-start this process and give it needed momentum, the federal government should empower a respected outside expert(s) in public service delivery to conduct a thorough, transparent review of public service IT systems and decision-making architecture to complement current internal efforts. Such a review would have three aims: first, better service delivery for Canadians; second, stronger internal public service proficiency and capacity; and third, a faster, deeper digital service transformation across government platforms. The United Kingdom undertook just such a review in 2010 — the Fox Review — which became the genesis of an internal public service embracing of digital government.
Once the results of this review are complete, a lead federal minister must be given the mandate to implement the required change across government. Making the radical changes necessary to both digital and management architecture will require the full support from the Office of the Prime Minister and the Privy Council Office, together with the help of a similarly empowered chief digital officer. A model for this approach could be taken from the United Kingdom, where Sir Francis Maude led widespread changes in his role of minister for cabinet office more than a decade ago.
Recommendation 2: Create more integrated and efficient data-sharing pathways
Throughout the conference, there was wide consensus about the value of data sharing for decision-makers, the public sector, academia, community leaders and the broader public. There was also a consensus about how this sharing of data between jurisdictions was a key challenge to Canada’s capacity to respond to the COVID crisis and to make key decisions.
The patchwork of rules that make up our data-governance structures is confusing and time-consuming to navigate. There is no universally agreed-upon set of rules, so those who want to access cross-jurisdictional data must invest resources and time to retrieve those data from 13 different governments with 13 different sets of regulations. When time is of the essence, this is far from optimal.
The main obstacle to better data sharing is not technological or privacy-related. It is cultural. A reluctance to share data is ingrained in our institutions. This report is not the first to raise this issue. Just recently an expert panel report of the Council of Canadian Academies (CCA), sponsored by Health Canada, came to similar conclusions (Council of Canadian Academies, 2023).
Panellists highlighted that part of the cultural and political barrier to data sharing rests on the fact that provincial governments fear their health-care information could be politicized and used against them. Consequently, for a better system of data sharing to emerge, it should not be driven by the federal government and should be separate from any accountability mechanism related to federal funding, such as the type of data-reporting requirements that recent FPT agreements in health care contain (e.g., Graefe & Fiorillo, 2023). Like the CCA, we believe a national approach to health data sharing cannot be successful if it is solely reliant on the leadership of the federal government. In this, we differ from the group of experts who recommended in the British Medical Journal (Bubela et al., 2023) that the federal government should compel governments to share data for pandemic preparedness.
There are examples of partial success in the data-sharing world such as the Canadian Institute for Health Information (CIHI). It has a governance structure that should alleviate provincial concerns and the expertise to play an expanded role in the data-production and data-sharing infrastructure of the country. We believe that an expanded role for CIHI or a similar organization devoted to data sharing is a better option than one that places the federal government at the centre. But provinces need to be fully committed. This is not just about sharing data to be compared once a year. This is about establishing pathways that would enable real-time sharing of data such as the epidemiological data required to respond to a crisis like the pandemic.
Recommendation 3: SYSTEMATICALLY EXAMINE PROCESSES AND STRUCTURES ACTIVATED DURING THE PANDEMIC
One essential exercise that every order of government should undertake is to systematically examine the processes and structures implemented during the pandemic and determine how these performed on three levels — increasing capacity, facilitating decision-making and engaging Canadians.
A second exercise should be to determine whether any of these processes and structures should become permanent fixtures for more resilient institutions and a more innovative and responsive government, or whether they can be activated rapidly when the situation requires it. Mining them for future emergency applications is good; examining them for current applications to build an improved government response is even better.
For instance, many governments established a COVID core committee or a COVID co-ordination committee, often grouping relevant departmental deputy ministers and other civil servants. These committees did not all have the same structure or the same mandate across the different governments. Some might have been better at generating integrated thinking and bringing together public health considerations with larger societal and economic impacts, something conference participants said was often lacking.
Delving into what worked well and what did not within these central co-ordination bodies is essential to responding to future crises. Ideally, this exercise would be done in a way that identifies best practices and produces conclusions that can be shared across all orders of government. It should be an exercise that makes learning possible within each government and across different orders of government.
Some of that work has been done, at least partially. For instance, the Ontario auditor general investigated the emergency management of the pandemic by the province, highlighting shortcomings and identifying best practices in other provinces. But the report also recommends that the province “determine the changes needed to make its provincial response structure as effective as possible, and implement them” (Office of the Auditor General of Ontario, 2020, p. 34). In other words, the hard work remains.
To repeat: these exercises should be done systematically within governments and the conclusions shared widely with senior public service officials at all levels.

COVID-19 was a significant challenge not just to Canadians, but to federalism itself. No single government had either the jurisdiction or the capacity to respond on its own. While each government had a role to play, collaboration, co-operation and co-ordination were necessary. Daily, we saw that unity of purpose and action could be achieved but was difficult to sustain. It was easy to come together for six months, but not for two years. When we think of federalism, we should not be hoping that future challenges are short and contained.
A lesson learned was that the intergovernmental institutions surrounding federalism can and do work. But this remained a process that was driven principally by executive federalism led by the first ministers themselves. They met more often in the first month of the pandemic than in the previous two years. This is not a sustainable or particularly wieldy mechanism, given its highly personal and political nature. In addition, this highly executive-driven process is by definition exclusive, confining itself to the two constitutional orders of government — federal and provincial/territorial — not the municipal or Indigenous self-governments that were essential in combating the virus.
A long-held virtue of Canadian federalism is its flexibility and innovation. Sub-national governments historically take different approaches to the same issue. Canadians generally accept this, leaving differences of opinion to the political process. But where do pandemics fit into that scenario? Because the responsibility for health-care delivery resides with provincial governments, premiers had a strong argument that they were on the front line of the response and emergency measures. But the front line for the virus was global not local, national not just provincial. Acting in concert was an essential tool in keeping COVID at bay. Clear and timely national guidance was essential. With multiple intergovernmental tables, coupled with multiple virus mutations, this proved difficult to generate, let alone maintain, over the long term.
Vaccine scarcity in the first part of 2021 created more divisions. Federal vaccine allocation formulas to provinces and territories proved fair, but it did not take long for daily scorecards of who had administered the most vaccines week by week to emerge. Competition replaced co-operation as governments raced to secure more and faster doses for their populations.
At the same time, the underlying federalism infrastructure chugged along, particularly in health care. Pre-existing health system co-operation agreements were exercised to transfer sick patients from one jurisdiction to another, to accommodate overflows. Medical personnel from one province helped in others as the virus ebbed and flowed. Genomic tracing of new virus strains was shared quickly across FPT public health units. Some lessons from SARS-1 in the early 2000s had clearly been learned and we hope some will be learned here again.
Recommendation 4: Identify intergovernmental structures that worked
As outlined above, the response to COVID-19 had a crucial intergovernmental component. However, this aspect of the response is not covered in reviews and reports produced by individual governments, like those done by auditors general for example.
Yet, in this realm, perhaps more than any other, it is important to identify the processes and structures that worked best. Given the centrality of FPT co-operation in a public health emergency, this seems obvious. For instance, there should be a thorough operational review of the different committees and working groups that were part of the FPT public health response plan for biological events. Were they all equally equipped to do their job? Did one format work better than another? Same questions for existing tables or conferences of FPT deputy ministers: How did they function? What was useful during a period of crisis and what wasn’t?
The main problem here is who should do this work. There has been very little examination of these processes across the different orders of government as our review of reports in Part I made clear, mostly because it is unclear who should or can do this work. As an institution, the Council of the Federation (COF) has neither the mandate nor the capacity. Operating by consensus bordering on unanimity, it would require all 13 premiers to direct such a study. Even then, historically, COF has not embarked upon such studies that could in any way result in unintended criticism, affecting their power of action, or being constrained institutionally by other provinces and territories.
Still, an examination of collaborative or co-ordinated efforts among provinces and territories — with or without the federal government — would serve federalism well. A similar examination by the federal government would have benefits, but a joint FPT examination would be the best-case scenario. The ideal format is likely to be a consortium of academic experts, policy specialists and former civil servants, tasked and funded by federal and provincial governments. Such an examination is essential to solidify our intergovernmental processes, especially at the departmental level.
It is impossible to predict what the next crisis will be, but we can comfortably predict it will require intergovernmental co-operation. We should make sure we learn from the COVID-19 experience and that we activate useful mechanisms when co-operation and co-ordination are needed.
Recommendation 5: Make intergovernmental relations more inclusive
Intergovernmental relations in Canada are heavily “executive-driven,” meaning they are dominated by discussions at the very top. This was even more true during the pandemic when the national aspect of the Canadian response came from the weekly meetings between first ministers.
One thing we heard multiple times during the conference was that other important actors in the pandemic response were left out of this process and/or were told what to do after the fact, with no particular time to provide meaningful input. Among those actors, two — municipalities and Indigenous governments — deserve more attention. We discuss Indigenous governments in more detail in Recommendation 6 given their unique constitutional status.
The inclusion of municipalities in intergovernmental relations during the pandemic varied across provinces, often relying on the personal connection between the premier and the mayors. This is not a workable system moving forward. Our institutions need to recognize that the role of municipalities in people’s lives and the Canadian federation has evolved and needs to be better reflected in how intergovernmental relations operate.
Our recommendation is not to include municipalities in existing formal forums of intergovernmental relations such as first ministers’ meetings or the Council of the Federation. After all, they are creatures of the provinces under the Canadian Constitution. However, we believe that the current intergovernmental relations framework needs to innovate and find other ways of including them in these discussions.
Research pointing to international experience and providing potential solutions exists (e.g. Eidelman, 2020; Hachard, 2022). We welcome more comparative work from academia on how other federations have included municipalities in intergovernmental relations, but the pandemic showed that it is time for the next step. It is time for actual initiatives to be put forward, and for governments to try different avenues.
Recommendation 6: Co-develop and formalize intergovernmental relations with Indigenous governments
Indigenous governments are governments, not stakeholders. Often, our national conversations about the federation fail to acknowledge that there is another constitutionally recognized order of government in Canada. Too often, as was the case in many instances during the pandemic, Indigenous governments were treated as outside interests lobbying for attention, rather than sovereign entities responsible for the health and well-being of their people.
For example, we heard that the inclusion of Indigenous governments in the decision-making process often happened late, varied greatly from one context to another, and was more ad hoc than deliberate and sustained. This is not meaningful inclusion, nor is it effective for the necessary on-the-ground response.
What meaningful inclusion looks like should be ascertained, co-developed with and implemented in co-operation with Indigenous governments across the country. These will be by necessity asymmetrical — as current federal/provincial/territorial relations are.
It is not for the authors of this report to declare what the mechanisms for those relationships should look like. However, at a minimum, the federal government should prioritize work on its action plan for the United Nations Declaration on the Rights of Indigenous Peoples Act, which lists as a goal: “Indigenous peoples enjoy and exercise the right to participate in decision-making in all matters that affect them.” Furthermore, the action plan commits to “strengthen Indigenous engagement by improving bilateral mechanisms with Indigenous partners [and] improve linkages between federal/provincial/territorial officials and Indigenous representatives across public health and health care systems.” (Government of Canada, n.d.)
Giving proper and practical constitutional meaning to this direction would alleviate the intergovernmental confusion and duplication that caused difficulties during the pandemic.
People who were in a decision-making position during the pandemic had to act fast in an ever-changing environment — one where complexity, risk and uncertainty were defining factors. The pandemic has receded but these factors remain. Whether we are talking about the impact of climate change or the domestic impact of wars abroad, many policy areas facing Canadian governments will be defined by a high level of uncertainty and a higher risk of being wrong and missing opportunities. They need to learn to better navigate this essential policy environment.
Recommendation 7: Incorporate positive risk-taking into public service processes to advance innovative ideas, improve service delivery and achieve better outcomes
The urgent need to respond to the pandemic required the usually risk-averse public service to take risks and be more innovative and imaginative. This meant that decisions had to be taken with incomplete information and short-circuited governance processes. In hindsight, some mistakes were made, but both action and responsiveness were necessary and demanded by Canadians.
A December 2023 report to the Clerk of the Privy Council on public service values and ethics clearly identified the risk-aversion problem: “Participants also discussed the culture of risk aversion that exists in the public service when it comes to providing fearless advice or giving dissenting opinions. They noted that the culture negatively impacts trust between employees and management, undermines creativity and innovation and decreases the level of overall trust and confidence in the system” (Government of Canada, 2023d, p. 19).
Unfortunately, one thing we overwhelmingly heard during the conference and in other conversations around this report is that the public service is already “snapping back” to the old ways of doing things. Allowing this to happen would be a lost opportunity. Governments must figure out how to institutionalize positive risk-taking into decision-making and governance processes. The conference heard how the relationship between public servants and elected officials became more fluid during the pandemic and that there was more open communication about errors and about how to correct course. We need to think hard about how we can continue to foster this type of dialogue, one where a shared public service and political culture of “fearless advice and loyal implementation” is routine.
Bringing about these types of changes is no easy task. It requires systems-level transformations and cultural change at both the public service and political levels. Nevertheless, some solutions are clear.
First, positive risk-taking must be encouraged at senior levels of government. Deputy ministers, senior executives and managers need to have the backs of their colleagues. Ministers need to take greater responsibility and show accountability for the decisions of their departments. The auditor general needs to recognize and not criticize risk-taking that is imperfect.
Second, innovation, positive risk-taking and agility need to be incentivized within internal governance processes. Treasury Board should require individual departments and agencies to undertake an active, positive risk-taking assessment of what they do and how they do it to identify specific barriers and opportunities. This includes approval processes, financial controls, decision hierarchies and other factors. Begin by assessing how each of these was approached differently during the pandemic and determine what changes could be institutionalized in normal times.
There is a clear recognition and appetite for this within the public service. A 2022 study by the IOG and the Brian Mulroney Institute of Government found that senior public servants, federally and provincially, were “unanimous in wanting to hold onto streamlined approval processes, flattened hierarchies, the relaxation of administrative, human resource and financial controls, and the use of interdisciplinary teams” (Institute on Governance & Brian Mulroney Institute of Government, 2022, p. 18). Undoubtedly some of the crisis measures will not be appropriate in normal governing times, but there are lessons to be learned about ways in which our public- sector institutions can be leaner and nimbler to enable risk-taking and innovation. That would improve service delivery, as well as policy and program outcomes for Canadians.
Third, debate and engagement within the public service must be actively encouraged to create a positive culture of risk-taking. Disagreement or dissenting opinions should not be viewed as threatening, disloyal or grounds for repercussions. Safe-space thinking out loud should be routine and rewarded.
Recommendation 8: Invest in the new leadership and operational skills development training needed and valued during the pandemic
One thing we heard clearly was that institutional performance during the pandemic depended on the people who worked tirelessly within those institutions. Resilience in our institutions relies in the first instance on the knowledge and skills of our public servants. A second thing we heard is that classical public administration skills focused on process were inadequate to the scope and imagination required to deal with the pandemic. Innovation, agility, adaptability and collaboration aimed at outcomes were more important and valuable. Finally, we heard that there is a need for the renewed importance of efficient, effective program and service delivery at the operational level. For provincial governments, closer to the front-line needs of citizens, this is not new. It is more of a stretch for the federal government. Post-pandemic service challenges in getting a passport on time or travelling through airports reinforces the need for a stronger internal focus and value being placed on this aspect of federal good governance.
Investing proactively to train public servants in these new essential skills will make our public institutions more resilient and better equipped to navigate through, and thrive in, an environment where risk, uncertainty and complexities will continue to be factors.
Specifically, we recommend investing in skills-development programming and courses for leaders and executives in the following key areas:
- Collaborative governance: Engaging and collaborating across government and with external stakeholders to devise and deliver more effective policies and programs
- Positive risk-taking and innovation: Identifying and assessing where risk-taking can be proactively incorporated into decision-making and service delivery
- Strategic foresight and planning: Building effective “over the horizon” capabilities to learn what issues, risks and opportunities need to be considered for the longer term
- Project management: Upgrading the management and technical skills for big project management delivery, particularly for IT, digital and data system transformation
Leaders within organizations need to champion this transformation. Investing in leadership development training is key to ensuring our public servants have the tools to do the jobs required. This is essential to build the public service we need, not just maintain the one we have.
Recommendation 9: Learn how to communicate policy uncertainty and complexity to Canadians
One roundtable participant mentioned that embedding a communication specialist within various scientific and public health teams would have been useful in crafting clearer messaging. We would take this recommendation in a different direction. It seems paramount that governments learn how to better communicate information in an uncertain environment. This starts by letting citizens know that there is uncertainty. Too often during the pandemic, spokespeople tried to convey a sense of certainty, perhaps out of caution. But this backfired when evidence evolved and required the message to change. The different recommendations over time about masking are perhaps the best example of this.
Decision-makers, specifically those who have to deliver messages to the people, need to trust that the audience will be able to live with uncertainty if it is communicated correctly. Transparency about uncertainty and trade-offs builds trust, as shown in the research of behavioural scientists such as Michael Bang Petersen (Bang Petersen et al., 2021).
Therefore, embed communication specialists within those teams — but not to craft a message that will make the government look good. What is needed is evidence-based messages, grounded in facts and data, that take into account how people cognitively deal with uncertainty.
We urge public health authorities and governments more generally to invest resources in this area. They should fund behavioural research around these questions, and consult and hire behavioural experts. The fellowship program of the impact and innovation unit (IIU) in the Privy Council Office is a good example that could be emulated by other governments.
Here, too, the media has a role to play. An immediate reflex by public actors calling out “backtracking,” shortchanges the public, who seek to understand the issues and how they should respond. COVID-19’s fast-moving and changing dynamics presented a perfect storm opportunity for public education, not just news reporting.
It is a brave politician or official who will publicly state “I don’t know.” Yet, when it came to COVID-19, this was manifestly true. We need to understand that, when politicians or experts communicate uncertainty, it does not mean they are indecisive. When their thinking on an issue evolves, it does not mean they were wrong in the first place or that they have “flip-flopped.” We expect governments to know things, but it is both unreasonable and impossible to expect them to know everything at once.
How uncertainty is communicated to the public matters for compliance and trust. When public health officials announced changes in public health measures, such as masking, it was depicted immediately by some politicians and the media as backtracking, clumsy and trust-eroding. This is not useful. This is not how science works.
From pandemics to climate change, science, data and evidence are all under challenge from actors outside governments. In a democracy, this is to be expected. But it is also being challenged within governments by officials seeking to know more from data and evidence, and to get it right for public policy responses.
Governments and their senior officials need to do a much better job of levelling with the public about what they know and what they don’t know about complex public policy issues. Perceived hiding of information or miscues in communicating science, evidence and trade-offs inevitably undermine public trust and confidence in government.

The landscape painted above — one that is marked by uncertainty, risk and complexity — is also one that needs to take into account what the pandemic did to the vivre ensemble. This was a clear message during the conference and one that has been a continuing refrain in this report. Trust was lost and we will not be able to face the next crisis if we do not rebuild it. There are two essential factors to rebuilding this trust — transparency and accountability.
Recommendation 10: Create a pan-Canadian task force to tackle misinformation and disinformation
The federal government has been delving into the nature and impact of disinformation — more so than any regional or local government. This makes sense, given that the federal government has more fiscal and human resources to carry out the work. For instance, the Privy Council Office’s Impact and Innovation Unit (IIU) has been conducting important cutting-edge research via large-scale surveys on trust, disinformation and misinformation.
However, to maximize its impact, this research should be shared with other orders of government regularly and efficiently. All other governments should be collaborating with the federal government on data collection and analysis. As is the case with any other complex policy challenge, valid, comprehensive and up-to-date data are essential to properly diagnose problems and identify potential solutions. Provincial, territorial, municipal and Indigenous governments need to be drawn into the federal data-collection process at the earliest opportunity so they can help identify the factors where we need more information. These include what topics are prone to the sharing of misinformation and disinformation and what factors lead to the increased consumption of misinformation and disinformation. After all, local and regional governments are more frequently in contact with members of the public through the delivery of programs and services. These governments have more regular opportunities to understand how disinformation and misinformation are affecting the public and where governments can help fill information gaps.
Perhaps more importantly, they are more likely to face the effects of a disinformed or misinformed public because they are more frequently communicating directly with their residents, whether that’s about programs and policies, services, public health announcements or anything involving evidence or science.
This is also true for knowledge and best practices on the behavioural side of things. Research has shown that many behavioural interventions worked well during the pandemic while others fell short (Ruggeri et al., 2024). Doing more of this research within governments and disseminating it more systematically across governments would help deal with future crises that require similar interventions.
This is why we believe creating a pan-Canadian task force on misinformation and disinformation that includes representatives from all orders of government is necessary. It would allow the identification and sharing of data on the determinants of susceptibility to disinformation and misinformation; sources of disinformation and misinformation; and ways for governments to combat this problem through the effective sharing of accurate, objective information. Further, the task force could help identify ways to nurture civic literacy so that citizens are more able to proactively practise “civic self-defence” and reject misinformation and disinformation. The task force could help institutionalize how data are shared across governments, ensuring that those who most need this knowledge have access to it. Canada has many experts in this field and this task force could act as a mechanism to bring these experts together and connect their work into the policy process.
Recommendation 11: Build inclusive and meaningful relationships with civil society leaders before the crisis hits
Whether it was the work done by physicians from the South Asian community in Brampton or Indigenous leaders and organizations in remote or urban settings, people trusted the messages coming from their own community leaders. The problem was that it took time for the established stakeholders and decision-makers to trust these leaders and give them the means necessary to do their part of the work. Trust is a two-way street. If governments do not trust community leaders, why should the opposite be true?
The pandemic made it clear that, in a moment of crisis, governments can’t be relied upon to do everything. They need to be able to count on people on the ground. Community responsiveness matters in a crisis and the civil society leaders who can make this happen need to be supported. Elected federal, provincial and municipal officials, as well as senior public servants, need to invest in these relationships now and find a way to build a governance model that is more horizontal than vertical. Engaging and collaborating with external stakeholders to devise and deliver more effective policies and programs should be a priority.
This is continuous work. These channels are much easier to activate when they have been developed over the years.
Recommendation 12: The Federal government should initiate a comprehensive pan-Canadian, collaborative lessons-learned examination
Our conference was the first public post-pandemic lessons-learned event. That is not good enough. In their desire to move on, governments have been hesitant or just plain unwilling to initiate any form of public accounting of how they responded to COVID-19. It’s easy to understand why. Emotions remain raw for many Canadians, while others just want to turn the page. Governments are therefore reluctant to stir things up again.
This, however, is short-sighted. There is value in systematically examining how our public institutions performed during the most demanding public health emergency of our time. We recognize that several governments have undertaken some form of review, as we set out in Part I. The federal government, meanwhile, has conducted its reviews within the public service in various departments, notably Health Canada, and has already begun to implement improvements. Auditors general have performed various accountability studies consistent with their retrospective lens on government processes, management and value for money.
However, none has considered a whole-of-government or pan-Canadian perspective. None can be relied upon to generate real lessons for our public institutions. However useful internally, no real case can be made they will prove sufficient in either their scope, depth or trust.
There are always risks with any form of public examination of controversial issues. Beyond the political risk to existing governments, which makes many of them reluctant to proceed, they can become lightning rods for disinformation about the most contentious decisions and moments of the pandemic. There is no guarantee our political actors will treat the process responsibly. Current divisions in the country could become deeper. None of this would serve Canadians well.
But the alternative does not serve Canadians well either. Failing to review how our public institutions performed, then failing to tell Canadians honestly and authentically what should be done, has a whiff of mediocrity and self-satisfaction about it. It subtracts from public confidence, rather than adds to it. It accepts mistrust with the public and does nothing to factually confront it at a time when a higher level of mistrust is a pandemic outcome itself.
We believe a public examination by governments of how public institutions performed and what lessons can be learned is manifestly in the public interest, but with caveats.
First, this should not be an open-ended blame game. That would simply reopen old grievances and hard feelings, and would not advance learning. It would also inhibit information sharing and helpful testimony, not enhance it.
Second, this should not be about looking backward, but looking forward. There is no real value in an inquiry that spotlights specific decisions at specific junctures to establish an official “truth.” The value is in how and why our public institutions performed a certain way and how they can be improved.
Third, led by experts, this panel should not be called an “inquiry” but an “examination.” This must not be an attempt at determining wrongdoing. There are no judicial principles or decisions at stake as the label of “inquiry” would suggest. Besides, formal inquiries are lengthy, expensive affairs that can frustrate the public, undermining the actual value of the process.
Here are five key components we recommend for such an examination. It should be:
- Focused: On public institutions’ performance across governments, not just the health system
- Collaborative: Canada’s pandemic response involved all governments, so all governments should be able to have input. But this should be initiated by the federal government.
- Public: Schedule hearings where community leaders and people who were involved with on-the-ground operations during the pandemic can listen and offer their perspectives
- Independent: Funded by government, reporting publicly to government, but managed and run on its own
- Expert: Led by (a) distinguished Canadian(s) with a history of public service outside partisan politics, supported by a panel of three to five experts in public health and public governance.
The mandate of this examination should be as follows:
“To examine and report publicly within two years on how Canada’s institutions of public health and public governance performed during the COVID-19 pandemic and derive lessons to be learned for improvements in preparedness, resilience, and performance by the public sector for Canadians.”
In a way, we are proposing something that has never been done, that governments, under the leadership of the federal government, create a joint panel reviewing institutional performance. The pandemic was a challenge like no other and we believe it calls for a lessons learned examination like no other.
Conclusion
You might not have heard of Dr. Raj Grewal but he is one of the heroes in the story of how Canada grappled with the COVID-19 pandemic. An emergency physician, Grewal watched in frustration in 2020 as Brampton, Ont., where he grew up, was ravaged by the virus and the usual regional and provincial institutions seemed unable to address the crisis.
“My community was on fire and we had to do something,” he said during a roundtable at our June 2023 conference. (Grewal agreed to have his comments put on the record.)
He and a group of other physicians came together to form the South Asian COVID Task Force. Through intense lobbying and resourcefulness, they established one of the largest testing sites in the country and ultimately got 100,000 residents vaccinated.
Brampton is a community with a large South Asian population where multiple generations share residences and many workers could not isolate effectively at home. The task force took to ethnic media outlets, created public health videos in Punjabi and lobbied the government to let it create vaccination centres in places where residents felt safe, such as the Embassy Grand Convention Centre and Banquet Hall.
Grewal’s story is inspiring but also raises a red flag for us. As one of our panellists noted earlier: “You cannot build resilient institutions solely around the dedication and professional heroism of public servants and community leaders.” It’s critical to find ways to strengthen our institutions to help combat the next crisis, whenever it comes.
Ultimately, Canada’s COVID-19 response hinged on governance. The response was only as good as our public institutions. That means there are key learnings to be drawn about how governments took decisions and who they involved; about how our federation worked when governments had to work together; and about how information flowed within and across governments and to Canadians.
We heard clearly during our Resilient Institutions conference that some of our key institutions were ill equipped to deal with a pandemic crisis that required strong communication channels and sophisticated data sharing, not just between levels of government, but with diverse communities having multiple needs. This report summarizes what was said, puts those conversations in context, and draws what we think are important lessons and recommendations.
Yet, we recognize that we’re only scratching the surface. Many of our recommendations call for more to be done: a task force on misinformation and disinformation; an exercise identifying intergovernmental structures that worked; and, crucially, a national lessons-learned examination spearheaded by governments.
Future studies and reports on Canada’s response to the pandemic should go above and beyond the public health dimension. Yes, the pandemic was a public health crisis. That is important. But its scope and scale impacted our whole society and economy. A narrow health focus would be inadequate in capturing all the lessons learned. The same can be said for a narrow focus on government spending during the pandemic.
We share this report as a call to action for governments and civil society to do more now before the natural inclination to “put this behind us” takes hold. It is crucial that our most important public institutions build resilience so they are ready for what comes next. We heard loud and clear at the conference that this discussion was important but was only just a first step. We hope others will read and act upon this report and take those necessary next steps.
Public Reports on COVID-19 from Governments
Appendix A: Public Reports on COVID-19 from Governments
Appendix B: Resilient Institutions Event Program
Public health decision-making during the pandemic
This roundtable will bring together individuals who played key roles in public health decision-making during the pandemic. Speakers will examine how decisions were made, whether existing governance structures and processes were sufficient and how new ones were adopted over time. They will also discuss what information is required for decision-making in a time of intense uncertainty, and how the public should be engaged in these decisions.
Panellists
Helen Angus — CEO, AMS Healthcare
Stephen Lucas — Deputy Minister of Health, Health Canada
Dr. Shannon McDonald — Former Chief Medical Officer, First Nations Health Authority
Dr. Fahad Razak — Internist, Unity Health Toronto, Epidemiologist, and Associate Professor, University of Toronto
Moderator
David McLaughlin — President and CEO, Institute on Governance
Data production and data sharing in the Canadian
health care system
The pandemic highlighted how crucial data is in informing health care decisions, and how it is imperative that we improve the sharing and use of data across Canada. This roundtable will bring together experts to explore lessons learned from the pandemic about data sharing in the health care system and identify how we can better collaborate across levels of government. The discussion will delve into the unique challenges and opportunities presented by Canada’s federal structure for data production and sharing, and suggest practical solutions for implementing best practices and bridging gaps exposed by the pandemic.
Panellists
Dr. Marcia Anderson — Dean of Indigenous Health, Social Justice and Anti-Racism and Executive Director, Indigenous Academic Affairs, Ongomiizwin-Indigenous Institute of Health and Healing, University of Manitoba
Anil Arora — Chief Statistician of Canada
Joanne Castonguay — Health and Welfare Commissioner, Government of Quebec
Glenda Yeates — Vice Chair, Canadian Blood Services
Moderator
Rob Annan — President and CEO, Genome Canada
Intergovernmental relations during the pandemic
The pandemic marked one of the most intense periods of intergovernmental relations in the country’s history. This roundtable will invite decision-makers to reflect on and share their real-life experiences during the pandemic. It will provide a deeper understanding of the challenges and opportunities presented by intergovernmental relations in times of crisis. In addition, the panel will consider how we can implement the aspects of intergovernmental relations that worked well during the pandemic to improve our response to future crises.
Panellists
Christiane Fox — Deputy Minister of Immigration, Refugees and Citizenship Canada
Stephen McNeil — Former Premier of Nova Scotia
Daniel Paré — Associate Deputy Minister, Department of Health and Social Service,
Government of Quebec
Kennedy Stewart — Former Mayor of Vancouver and Associate Professor, Simon Fraser University School of Public Policy
Moderator
Catherine Cullen — Senior Reporter, CBC
Imagining a federal community that works
The pandemic highlighted the strengths and weaknesses of Canada’s federation. Bringing together senior civil servants, elected officials and private sector representatives, this roundtable will consider how we can better co-ordinate and collaborate across levels of government to build a more resilient and responsive federation. What do our current institutions do well? How can they improve? How can we better leverage the expertise and resources of all levels of government to ensure an effective response to future crises? Responses to these questions are an essential step in making sure that Canada is ready for the challenges ahead.
Panellists
Jesse McCormick — Senior Vice President, Research Innovation and Legal Affairs, First Nations Major Projects Coalition
Carole Saab — Chief Executive Officer, Federation of Canadian Municipalities
Michael Vandergrift — Deputy Minister, Intergovernmental Affairs and Deputy Secretary to the Federal Cabinet
Mike Gladstone — Director, External Affairs, Enbridge Canada
Coleen Volk — Former Deputy Minister of Intergovernmental Relations and Associate Deputy Minister of the Executive Council for the Government of Alberta
Moderator
Charles Breton — Executive Director, Centre for Excellence on the Canadian Federation
Keynote Address: BUILDING AN ADAPTABLE COUNTRY
Countries that want to thrive in this turbulent century must be adaptable. They must be good at reconfiguring public institutions to meet new challenges and evolving public expectations. Our challenge is demonstrating that Western democracies like Canada can be as nimble under stress as technocratic authoritarian systems like China.
Contrary to conventional wisdom, Canada has a good track record on adaptability. Its governmental system has been transformed over the last 40 years. Distinctive features of the Canadian approach to governing, including heavy investment in forward thinking and concern for protecting the public sphere, allowed the country to respond effectively to new conditions and ideas.
In this century, however, adaptability is under threat. We have shifted our focus toward short-term politics and away from forward thinking. Technological change has disrupted the public sphere. And our public services appear less nimble. We need a program of reform that is focused on improving our flexibility for the dangerous decades ahead.
Panellist
Alasdair Roberts — Professor of Public Policy, University of Massachusetts, Amherst
Public service delivery and governance
Bringing together experienced voices from inside and outside the public service, this roundtable will reflect on public service governance and service delivery during the pandemic. How did public services adapt during the pandemic? In what ways did public service delivery change? The roundtable will explore obstacles to public service delivery adaptation and how they were overcome. It will draw key governance lessons to improve public service delivery outcomes for Canadians.
Panellists
Neil Bouwer — Visiting Professor of Practice, Max Bell School of Public Policy, McGill University
Graham Flack — Secretary, Treasury Board of Canada Secretariat
Lori Wanamaker — Vice Chair, BC Hydro and former Clerk, B.C. Government
Michael Wernick — Jarislowsky Chair in Public Sector Management, University of Ottawa
Public servants’ roles and skills for tomorrow
What does the future of our public service look like and how did the digital shift during the pandemic alter governments’ ability to deliver services? This roundtable will consider the public service of tomorrow and how it can be more agile, adaptable and digitally focused. It will discuss what skills and training Canada’s public servants will need to meet postpandemic demands.
Panellists
Amanda Clarke — Associate Professor, School of Public Policy and Administration, Carleton University
Taki Sarantakis — President of the Canada School of Public Service
Catrina Tapley — Former Deputy Minister of Immigration, Refugees and Citizenship Canada
Ryan Androsoff — CEO and Founder, Think Digital
Stephen Harrington — National Lead of Workforce Strategy, Deloitte
Moderator
Charelle Evelyn — Managing Editor, The Hill Times
The public’s experience of dealing with institutions during COVID-19
An analysis of the country’s pandemic response needs to consider the views and experiences of the broader population as well as those at the heart of it. This roundtable will bring together those with on-the-ground knowledge of how various groups were affected by the pandemic. They will examine how institutions performed during the pandemic from that point of view and identify how we can ensure that the voices and experiences of the public are not overlooked in the decision-making process. The roundtable will allow us to explore potential solutions for more effective and inclusive institutions that better meet the diverse needs of communities.
Panellists
Jocelyn Formsma — Chief Executive Officer, National Association of Friendship Centres
Dan Kelly — President and CEO, Canadian Federation of Independent Business
John McAndrews — Managing Director, Digital Society Lab, McMaster University
Dr. Raj Grewal — Emergency Physician in Hamilton and Co-Founder of the South Asian COVID-19 Task Force
Moderator
Charles Breton — Executive Director, Centre of Excellence on the Canadian Federation
Trust, communication and decision-making
This roundtable will consist of elected officials, commentators and academics who will reflect on how our democratic institutions performed during the pandemic, focusing on public trust and communications. It will consider how the trust of citizens can be restored and our democratic institutions made more resilient. It will also seek ways to foster a stronger relationship between elected officials, governments and citizens in the future.
Panellists
Shachi Kurl — President, Angus Reid Institute
Isabelle Mondou — Deputy Minister, Canadian Heritage
The Honourable Erin O’Toole, MP — Former Leader of the Official Opposition
Lori Turnbull — Director, School of Public Administration and Associate Professor of Political Science, Dalhousie University
Moderator
Jennifer Ditchburn — President & CEO, IRPP
Land Acknowledgment
Monique Manatch
References
Adach, K. (2020, December 2021). A ministry steeped in traditional goes virtual. Public Policy Forum. https://ppforum.ca/wp-content/uploads/2020/12/C7-MAG-PPF-Dec2020-ENG.pdf
Angus, H. (2023, June 6). What was different about Ontario’s COVID-19 response. Policy Options.
https://policyoptions.irpp.org/magazines/june-2023/ontario-covid-19-response-plan-lessons/
Auditor General of New Brunswick. (2023, September). Volume I performance audit.
https://www.agnb-vgnb.ca/content/dam/agnb-vgnb/pdf/Reports-Rapports/2023V1/Agrepe.pdf
Bang Petersen, M., Bor, A., Jørgensen, F., & Lindholt, M. F. (2021). Transparent communication about negative features of COVID-19 vaccines decreases acceptance but increases trust. Proceedings of the National Academy of Sciences, 118(29), Article e2024597118.
https://doi.org/10.1073/pnas.2024597118
Blais, A., Howell, G., Tóth-Király, I., & Houle, S. (2023). Profiles of burnout and work engagement in a public service organization: Nature, drivers, and outcomes. Health Reports.
https://www.doi.org/10.25318/82-003-x202301200001-eng
Boots, S. (2023, November 29). Revolution, not evolution, for federal public service delivery [YouTube video]. Presentation at FWD50 2023.
Breton, C., Han, J., Tabbara, M., & Sim, P. (2021). COVID-19 Canadian provinces measures dataset. Centre of Excellence on the Canadian Federation.
Bubela, T., Flood, C. M., McGrail, K., Straus, S. E., & Mishra, S. (2023). How Canada’s decentralised covid-19 response affected public health data and decision making. BMJ, 382, Article e075665.
https://www.doi.org/10.1136/bmj-2023-075665
Canadian Institute for Health Information. (n.d.-a). Impact of COVID-19 on Canada’s health care systems: COVID-19’s impact on long-term care. CIHI. https://www.cihi.ca/en/covid-19-resources/impact-of-covid-19-on-canadas-health-care-systems/long-term-care
Canadian Institute for Health Information. (n.d.-b). Explore wait times for priority procedures across Canada. CIHI. https://www.cihi.ca/en/explore-wait-times-for-priority-procedures-across-canada
Canadian Institute for Health Information. (2022). About CIHI. CIHI. https://www.cihi.ca/en/about-cihi
Canadian Institute for Health Information. (2023). Taking the pulse: A snapshot of Canadian health care 2023. CIHI. https://www.cihi.ca/en/taking-the-pulse-a-snapshot-of-canadian-health-care-2023
Cassola, A., Fafard, P., Nagi, R., & Hoffman, S. J. (2022). Tensions and opportunities in the roles of senior public health officials in Canada: A qualitative study. Health Policy, 126, 988–995.
https://doi.org/10.1016/j.healthpol.2022.07.009
Champagne, E., Choinière, O., & Granja, D. (2023). Government of Canada’s teleworking and hybrid policies in the aftermath of the COVID-19 pandemic. Canadian Public Administration, 66, 158-175. https://doi.org/10.1111/capa.12520
Clarke, A. (2023, June 12). Who’s going to finally fix federal public service management? Policy Options. https://policyoptions.irpp.org/magazines/june-2023/public-service-management/
Council of Canadian Academies. (2023). Connecting the dots. Expert Panel on Health Data Sharing, CCA. https://cca-reports.ca/wp-content/uploads/2023/10/Connecting-the-Dots_ENdigital_FINAL.pdf
de Faye, B., Perrin, D., & Trumpy, C. (2022, September 23). COVID-19 lessons learned review final report. https://www2.gov.bc.ca/assets/gov/public-safety-and-emergency-services/emergency-preparedness-response-recovery/embc/reports/covid-19_lessons_learned_report.pdf
Eidelman, G. (2020). Reimagining the Canadian federation through an urban lens. Essay No 6. Institute for Research on Public Policy.
Ekos Politics. (2022). Public attitude to the “Freedom Movement.” https://www.ekospolitics.com/index.php/2022/09/public-attitudes-to-the-freedom-movement/
Fafard, P., Wilson, L. A., Cassola, A., & Hoffman, S. J. (2020). Communication about COVID-19 from Canadian provincial chief medical officers of health: A qualitative study. CMAJ Open, 8(3), E560-E567. https://doi.org/10.9778/cmajo.20200110
First Nations Health Authority. (n.d.). FNHA overview. https://www.fnha.ca/about/fnha-overview
Government of Canada. (n.d.). United Nations Declaration on the Rights of Indigenous Peoples Act: Action plan 2023-2028. Department of Justice Canada. https://www.justice.gc.ca/eng/declaration/ap-pa/index.html
Government of Canada. (2020). Safe Restart Agreement. https://www.canada.ca/en/intergovernmental-affairs/services/safe-restart-agreement.html
Government of Canada. (2022). Federal-provincial-territorial public health response plan for ongoing management of COVID-19. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/federal-provincial-territorial-public-health-response-plan-ongoing-management-covid-19.html
Government of Canada. (2023a). COVID-19 vaccines and Indigenous peoples.
https://www.sac-isc.gc.ca/eng/1606941379837/1606941507767
Government of Canada. (2023b). COVID-19 vaccination: Vaccination coverage.
https://health-infobase.canada.ca/covid-19/vaccination-coverage/
Government of Canada. (2023c). COVID-19 vaccination: Doses distributed.
https://health-infobase.canada.ca/covid-19/vaccine-distribution/
Government of Canada. (2023d). Deputy Ministers’ Task Team on Values and Ethics report to the Clerk of the Privy Council. https://www.canada.ca/en/privy-council/services/publications/deputy-ministers-task-team-values-ethics-report-clerk-privy-council.html
Government of Canada. (2023e). Sessional paper 8555-441-2022. Response to MP Wagantall, Yorkton-Melville.
Graefe, P., & Fiorillo, N. (2023). The federal spending power in the Trudeau era: Back to the future? IRPP Study No. 91. Institute for Research on Public Policy.
Hachard, T. (2022, May 17). A seat at the table: Municipalities and intergovernmental relations in Canada. IMFG. https://tspace.library.utoronto.ca/bitstream/1807/111338/1/imfgpaper_no59_intergovernmental_tomashachard_may_17_2022.pdf
Han, J., & Breton, C. (2022, February 1). Have provinces put schools first during COVID? Policy Options.
https://policyoptions.irpp.org/magazines/february-2022/have-provinces-put-schools-first-during-covid/
Indigenous Services Canada. (n.d.). Indigenous health care in Canada. Government of Canada. Retrieved from https://www.sac-isc.gc.ca/eng/1626810177053/1626810219482
Indigenous Services Canada. (2020, July). Update on COVID-19 in Indigenous communities. Government of Canada. https://www.canada.ca/en/indigenous-services-canada/news/2020/07/update-on-covid-19-in-indigenous-communities0.html
Institute on Governance. (2023, May 26). Trust in government. Action Learning Project.
https://iog.ca/wp-content/uploads/2023/05/Trust-Paper-Final_CW_May-26-2023.pdf
Institute on Governance & Brian Mulroney Institute of Government. (2022, May). Top of mind: Answering the call, adapting to change. Summary report: https://iog.ca/wp-content/uploads/2022/05/Top-of-Mind-Summary-Report-EN.pdf
Johns Hopkins University. (n.d.). Mortality analyses. Johns Hopkins Coronavirus Resource Center.
https://coronavirus.jhu.edu/data/mortality
Katz, A., Enns, J., Wong, S. T., Williamson, T., Singer, A., McGrail, K., Bakal, J. A., Taylor, C., & Peterson, S. (2018). Challenges associated with cross-jurisdictional analyses using administrative health data and primary care electronic medical records in Canada. International Journal of Population Data Science, 3(3), Article 6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8142948/pdf/ijpds-03-437.pdf
Mallard, A., Pesantes, M. A., Zavaleta-Cortijo, C., & Ward, J. (2021). An urgent call to collect data related to COVID-19 and Indigenous populations globally. BMJ Global Health, 6(3), Article e008847.
https://gh.bmj.com/content/6/3/e004655
Manning, P., Kelly-Gagnon, M., Major, J. C., Mintz, J. M., Fulford, M., & Tanguay, R. (2023, November 7). Public Health Emergencies Governance Review Panel final report. https://open.alberta.ca/dataset/dae4329f-265c-4b1f-adb4-3c6fdcf9eef1/resource/fb329cb6-aeb8-4cde-bf33-79a6fa20ac93/download/jus-public-health-emergencies-governance-review-panel-final-report.pdf
May, K. (2022, April 7). Some public service executives ‘burned out’ by crisis management. Policy Options. https://policyoptions.irpp.org/magazines/april-2022/some-public-service-executives-burned-out-by-crisis-management/
McAndrews, J., Beyer, A., & van der Linden, C. (2023, June 8). Who the public trusted during the pandemic. Policy Options. https://policyoptions.irpp.org/magazines/public-trust-canadian-institutions-covid-19/
OECD. (2023). Health at a glance: Canada. Organisation for Economic Co-operation and Development. https://www.oecd.org/canada/health-at-a-glance-Canada-EN.pdf
Office of the Auditor General of Canada. (n.d.). What we do.
https://www.oag-bvg.gc.ca/internet/english/au_fs_e_371.html
Office of the Auditor General of Ontario. (2020). Special report: COVID-19 pandemic — Chapter 1: Emergency Management Ontario. https://www.auditor.on.ca/en/content/specialreports/specialreports/COVID-19_ch1EMO_en20.pdf
Office of the Prime Minister. (2020, January 27). Prime Minister Justin Trudeau meets with the Incident Response Group. Prime Minister of Canada. https://www.pm.gc.ca/en/news/readouts/2020/01/27/prime-minister-justin-trudeau-meets-incident-response-group
Office of the Prime Minister. (2021, December 14). Prime Minister Justin Trudeau holds 35th call with Premiers on COVID-19 response. https://www.pm.gc.ca/en/news/readouts/2021/12/14/prime-minister-justin-trudeau-holds-35th-call-premiers-covid-19-response
Our World in Data. (2024). Share of people who completed the initial COVID-19 vaccination protocol [data set]. Our World in Data. https://ourworldindata.org/grapher/share-people-fully-vaccinated-covid
Pan-Canadian Public Health Network. (2023). COVID-19 response. https://phn-rsp.ca/en/about/covid-19-response.html
Public Health Agency of Canada. (n.d.). Public Health Agency of Canada. Government of Canada.
https://www.canada.ca/en/public-health.html
Public Health Agency of Canada. (2003, October). Learning from SARS: Renewal of public health in Canada — A report of the National Advisory Committee on SARS and Public Health.
https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/publicat/sars-sras/pdf/sars-e.pdf
Public Health Agency of Canada. (2017). Federal/provincial/territorial public health response plan for biological events. Government of Canada. https://www.canada.ca/en/public-health/services/emergency-preparedness/public-health-response-plan-biological-events.html
Public Health Agency of Canada. (2020). Lessons learned from the Public Health Agency of Canada’s COVID-19 response (Phase One). https://ourcommons.azureedge.net/data/Motion2020-10-26/2021-01-20-SPDP-8550-432-1-01/HESA_PHAC-ASPC_0000186_E.pdf
Razak, F., Shin, S., Naylor, C. D., & Slutsky, A. S. (2022). Canada’s response to the initial 2 years of the COVID-19 pandemic: A comparison with peer countries. Canadian Medical Association Journal, 194(25), E870-E877. https://doi.org/10.1503/cmaj.220316
Ruggeri, K., Stock, F., Haslam, S. A., Capraro, V., Boggio, P., Ellemers, N., Cichocka, A., Douglas, K. M., Rand, D. G., van der Linden, S., Cikara, M., Finkel, E. J., Druckman, J. N., Wohl, M. J. A., Petty, R. E., Tucker, J. A., Shariff, A., Gelfand, M., Packer, D., … Willer, R.. (2024). A synthesis of evidence for policy from behavioural science during COVID-19. Nature, 625, 134-147. https://doi.org/10.1038/s41586-023-06840-9
Shared Services Canada. (2021). One year into COVID-19. https://www.canada.ca/en/shared-services/corporate/publications/ssc-one-year-into-covid-19.html
Smylie, J., McConkey, S., Rachlis, B., Avery, L., Mecredy, G., Brar, R., Bourgeois, C., Dokis, B., Vandevenne, S., & Rotondi, M. A. (2022). Uncovering SARS-COV-2 vaccine uptake and COVID-19 impacts among First Nations, Inuit and Métis Peoples living in Toronto and London, Ontario. Canadian Medical Association Journal, 194(29), E1018-E1026. https://www.cmaj.ca/content/194/29/E1018#sec-14
Statistics Canada. (n.d.). Health statistics. https://www.statcan.gc.ca/en/subjects-start/health
Statistics Canada. (2022a). COVID-19 in Canada: A two-year update on social and economic impacts. https://www150.statcan.gc.ca/n1/pub/11-631-x/11-631-x2022001-eng.htm
Statistics Canada. (2022b). Government spending by function, 2021. The Daily.
https://www150.statcan.gc.ca/n1/daily-quotidien/221125/dq221125a-eng.htm
Tam, T. (2018). Fifteen years post-SARS: Key milestones in Canada’s public health emergency response. Canada Communicable Disease Report, 44(5), 98-101. https://doi.org/10.14745/ccdr.v44i05a01
Tripp, L. (2022). Overlooking the Canadian Indigenous demographic data: A response to Mallard et al’s call for data on COVID-19 and Indigenous populations. BMJ Global Health, 7(3), Article e008847. https://gh.bmj.com/content/7/3/e008847
Turnbull, L. (2023, June 9). ‘Winner-take-all’ politics threatens Canadian democracy. Policy Options. https://policyoptions.irpp.org/magazines/june-2023/winner-take-all-politics/
University of Manitoba. (n.d.). The Manitoba population research data repository. Retrieved from
https://umanitoba.ca/manitoba-centre-for-health-policy/data-repository
Varner, C. (2023). Emergency departments are in crisis now and for the foreseeable future. Canadian Medical Association Journal, 195(24), E851-E852. https://doi.org/10.1503/cmaj.230719
Wernick, M. (2023, June 6). Stress testing Canadian governance. Policy Options.
https://policyoptions.irpp.org/magazines/june-2023/stress-testing-canadian-governance/
World Health Organization (WHO). (2023). WHO COVID-19 dashboard [original data].
https://data.who.int/dashboards/covid19/cases?n=c
Wu, C., Bierman, A., & Schieman, S. (2022). Socioeconomic stratification and trajectories of social trust during COVID-19. Social Science Research, 108, Article 102750.
https://www.sciencedirect.com/science/article/pii/S0049089X22000564